CELLULAR ADAPTATIONS OF GROWTH AND DIFFERENTIATION
advertisement

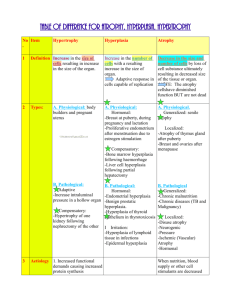
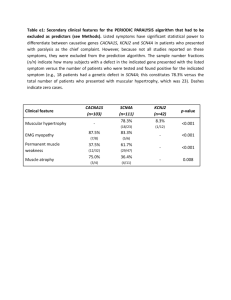
CELLULAR ADAPTATIONS OF GROWTH AND DIFFERENTIATION In order to function properly, the cells and tissues have to maintain a steady state (homeostasis)- the cells must constantly adapt cellular adaptation- is the state between a normal unstressed cell and the overstressed injured cell -by definition - an adaptative process is reversible -within defined limits, all the cells are capable of adapting to a variety of stimuli which may upset normality NORMAL CELL GROWTH -Normal tissue growth depends on a balance between the number of cells actively dividing and the number of the cells dying -the cells of the body can be divided into 3 groups on the basis of their regenerative capacity- they respond differently to stress and injury 1.- Labile cell ( intermitotic) 2.- Stable cell ( reversible postmitotic ) 3.- Permanent cell ( irreversible postmitotic) The cell cycle and types of cells Proliferating cells occupy several functional states between two mitoses. The cell cycle consists of G1 gap (presynthetic), S (DNA synthesis), G2 gap (premitotic) and M (mitotic ) phases. The cells may leave cell cycle during G1 and then they either cease proliferation, differentiate or eventually die or they enter G0 phase, resting phase from which they can be eventually recruited back to the cycle. G0 phase is a non-proliferative and is known as growth arrest 1.- Labile cells- continuously dividing cells- they continue to proliferate, remain all the time in cell cycle -tissues that contain most labile cells include-epithelia such as -stratified squamous epithelium of the skin, oral cavity, vagina cervix, esophagus, -lining epithelial cell of the gland such as salivary glands, pancreas biliary tract, -columnar epithelium of uterus, fallopian tube, -urinary epithelium -lymphoid tissue, hematopoetic tissue 1 2.-Stable cells- quiescent- they are considered to be in G0 phase, may undergo rapid proliferation after appropriate stimuli, they may be recruited back to the cell cycle stable cells include: -parenchymal cell of virtually all glandular organs, such as liver, kidney, pancreas, breast, lung -mesenchymal cells, such as fibroblasts and smooth muscle cells -vascular endothelial cells 3.- Permanent cells- non-dividing. These cells have left cell cycle and cannot undergo mitotic division. This group includes: -nerve cells -skeletal and heart muscle cells These cells have no regenerative capacity. Most tissues consist of mixture of all 3 cell types- for example the brain contains of neurons-permanent cells, and astrocytes- stable cells, etc. -the ability of cells to divide is linked with their reaction to injury -labile and stable cells can quickly replace dead cells- by exactly the same cells- the process is called regeneration -permanent cells by definition cannot divide and are not able to replace lost cells by the same cell type - instead repair occurs- dead tissue is removed and replaced by scar (collagen) CONTROL OF THE CELL CYCLE -growth factors and cyclins- the major classes of proteins in cellcycle regulation growth factors- low-molecular-weight proteins which have similar mechanism of activity as hormones -growth factors are produced by the cells and act either on the cell itself (autocrine activity) or an the neighbouring cells (paracrine action) by linking to cell surface receptors cyclins- are a family of proteins which seem to coordinate the journey of the cells through different parts of the cell-cycle CELLULAR ADAPTATION under normal conditions=physiologic adaptation -include responses to normal stimuli by hormones, cytokines, various endogenous chemical substances examples: enlargment of breast during pregnancy and lactation period, shrinkage of testes and ovaries with the age 2 under pathologic conditions=pathologic adaptation There are four main adaptative states: 1.-atrophy- shrinkage of the organ as a result of decreased cell size or/and the cell number 2.-hypertrophy - enlargment of the organ as a result of increased cell size 3.-hyperplasia - enlargment of the organ as a result of increased cell number 4.-metaplasia -the replacement of one cell type by another cell type in a tissue or organ 1. ATROPHY - is a decrease in the size of tissue or organ resulting from decrease either in the size of individual cells or in the number of cells composing the tissue atrophy- decrease in size of normally developed organ. It is different from agenesis, aplasia, hypoplasia which are abnormalities of organ development. atrophy- decrease in the size of the cell results from the loss or reduction of cell substances, reduction of the number of cytoplasmic organelles associated with diminished cell function Atrophy represents a reduction of cell structural components -less mitochondria -less endoplasmic reticulum -fewer myofilaments metabolic rate is reduced -less amino acid uptake -less oxygen consumption -less protein synthesis Degenerating organelles are taken up in lysosomal vacuoles for enzymatic digestion, process is represented by -marked increase in the number of autophagic vacuoles -many autophagic vacuoles may resist digestion—residual bodies some of them contain lipofuscin granules-brown atrophy -atrophy may progress to cell injury and death, a decrease number results from cell death due to irreversible cell injury sufficient number of cells is involved-the entire tissue or diminishes in size= becomes atrophic - connective tissue or adipose fills partly tissue defect due to atrophy in cell -when organ tissue 3 CLASSIFICATION OF ATROPHIES 1. Atrophy of disuse - decreased workload this type of atrophy occurs for example in immobilized skeletal muscle and bone when fractured limb is put into the cast. Skeletal muscle atrophies quite rapidly -atrophy is initially the result of rapid decrease in the size of cells, which is reversible if the muscles become active again. -Prolonged immobilization results, however, also in decrease of number of muscle fibers. Since skeletal muscle can regenerate only to a limited extent, restoration of muscle size can only occur through compensatory hypertrophy of the surviving fibers. -atrophy of bone- when bone resorption occurs more rapidly than bone formation= osteroporosis 2.denervation atrophy - loss of inervation -good example for this type of atrophy is skeletal muscle. Skeletal muscle is dependent on its nerve supply for normal function and size: Damage to motor neuron at any point leads to rapid atrophy of muscle fibers. Denervation can be temporary- normal function can be restored when nerve continuity is reestablished. 3.vascular atrophy - caused by a diminished vascular blood supplyischemia- results in atrophy due to progressive cell loss. for example- vascular atrophy of kidney in atherosclerosis 4. atrophy due to loss of hormonal stimuli -endometrium, breast, many endocrine glands, prostate are dependent on trophic hormones for normal cellular growth -withdrawal leads to atrophy of target cells -there is an example of iatrogenic atrophy: -high dose of corticosteroid therapy (commonly used for immunosupression) may cause atrophy of adrenal glands (because of decrease of secretion of ACTH by pituitary gland)- these patients lose ability to secret corticosteroid - after withdrawal of drugs- crisis may occur caused by a low level of endogenous secretion of corticoids 5. Atrophy due to lack of nutritional supply -severe protein-calarie malnutrition= marasmus adipose tissue is used, exhausted, then skeletal muscle and other organs are used as sources of energy and proteins- marked muscle atrophy 6. senile atrophycell loss is one of the morphological changes in aging most apparent in organs composed of permanent cells (brain, heart) - no capacity to regenerate less apparent - in tissues with higher ability to regenerate 4 2. HYPERTROPHY =increase in the size of individual cells - if sufficient number of cells is involved-increase in size of the entire organ hypertrophied organ has no new cells, but larger ones Hypertrophy represents: -synthesis of more membranes -more ATP, more enzymes, more cytoskeletal filaments, ribosomes, Golgi zones - in muscle fibers - increase in size of cytoplasmic myofibrils hypertrophy is mainly seen in cells which have no capacity for mitotic division- skeletal muscle, heart muscle -physiologic hypertrophy - hypertrophy may occur as an adaptation to increased demand or to specific hormonal stimuli. Hypertrophy is controlled response reflecting an increased demand, if the demand is removed, the tissue can revert toward normal for example -hormone stimulation-growth of uterus during pregnancy -increased workload- bodybuilder skeletal muscle -pathologic hypertrophy - abnormal ( pathologic ) hypertrophy occurs in the absence of an appropriate stimuli of increased demand, usually does not revert back to normal for example: -increased resistence- cardiac hypertrophy in high blood pressure -bladder muscle hypertrophy- in outflow obstruction to urine caused by an enlarged prostate the best example of adaptative hypertrophy occurs in the heart in a variety of diseases= myocardial hypertrophy -hypertension = high blood pressure- the heart must contract against higher pressure in the aorta-the heart achieves weighs more than normal 350 g -whatever the mechanism of hypertrophy is- it can reach limits of adaptation— -enlargment of the myofibres is no longer able to compensate the work overload - and cardiac failure follows -at this stage- degenerative changes in cardiac muscle fibers limiting factors of hypertrophy are poorly understood—may be due to limited blood supply to enlarged fibers 3. HYPERPLASIA -increase in number of cells in organ or tissue which may thus increase its volume 5 Hypertrophia and hyperplasia- closely related, they often develop concurently -Hyperplasia can occur only in cell population capable of dividing (synthesis of DNA, thus permitting cell division) regeneration after loss of tissue, depends on regenerative capacity of cell capacity for hyperplastic growth-depends on cell type: high capacity - epidermis, intestinal epithelium, hepatocytes, fibroblasts, bone marrow cells etc low or no capacity-nerve cell, skeletal and cardiac muscle intermediate capacity-bone, cartilage, smooth muscle more details on this topic- next lecture on regeneration, repair and wound healing hyperplasia -physiological causes of hyperplasia -hormonal -proliferation of glandular epithelium in female breast at puberty and during pregnancy -hyperplasia in pregnant uterus -cell loss- regeneration of the liver after partial hepatectomy - regeneration of squamous epithelium in wound healing -compensatory - hyperplasia of one kidney associated with developmental hypoplasia of the other one -pathological causes of hyperplasia hormonal -endometrial hyperplasia- is an important result of increased estrogen stimulation typically occurs in menopause (when estrogen is not opposed by progesteron secretion)- endometrial hyperplasia is associated with irregular, often excessive uterine bleedingendometrial hyperplasia may progress into atypical hyperplasiasignificantly higher risk of cancer -thyroid hyperplasia (goiter)- most important is Graves disease (Basedow disease) results from increased stimulation of TSH- stimulated thyroid to higher secretion of thyroxin -hyperplasia of prostate gland- common in older men due to hyperplasia both the glandular and the stromal elements- cause of hyperplasia- increased sensitivity of smooth muscle of the prostate to estrogen stimulation (due to decrease of androgen activity) -cell destruction- in ulcerative colitis- the colonic mucosa undergoes repeated ulcerations, cell loss and regeneration and hyperplasia 4. METAPLASIA 6 -is an abnormality of cell differentiation in which one type of mature cell is replaced by a different type of adult cell - the latter one (metaplastic ) is not normal for the involved tissue -metaplasia results from abnormal differentiation of stem cell -metaplasia is reversible involves most often epithelium- the germinative (stem) cells multiply rapidly and differentiate in abnormal manner - stem cells are usually present adjacent to BM. Epithelial metaplasia is thus a manifestation of varied potential for differentiation in stem cells. typically occurs in chronic inflammation Types of metaplastic changes: -squamous metaplasia - the most common type of epithelial metaplasia nonsquamous columnar or pseudostratified epithelium is replaced by stratified squamous epithelium -squamous m. is common in the uterine cervix, in the bronchial mucosa, in chronic inflammation of nasal cavity and paranasal sinuses - Clinical significance: in bronchi- loss of cilia in normal respiratory epithelium predispose to development of chronic inflammation -glandular metaplasia - occurs in the esophagus, where the normal epithelium is replaced by glandular mucus secreting epithelium (either of gastric of intestinal type)= Barret esophagus Clinical significance: risk of delevopment of peptic ulcer in metaplastic gastric mucosa -intestinal metaplasia - occurs often in chronic gastritis Metaplasia only rarely occurs in mesenchymal tissue: -osseous metaplasia - in scars 7