Atrioventricular and Intraventricular
advertisement

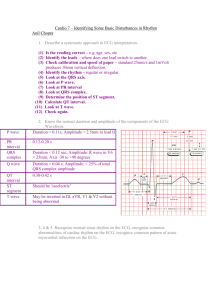
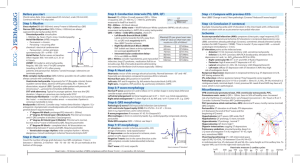
Conduction Defects Atrioventricular and Intraventricular 1 Sick Sinus Syndrome One subset is tachy-brady syndrome Alternating periods of long pauses/bradycardia with supraventricular tachyarrhythmias (afib, flutter, SVT) Causes are multiple; medications used to control tachyarrhythmias worsen pauses. Therapy is PPM with meds for rate control 2 A-V conduction defects 3 First Degree AV block Fixed, prolonged PR interval (>0.20 sec) Can be as long as 0.60 sec. Found in normals with increased vagal tone, meds (digoxin, Ca Channel blockers, Beta blockers), and occasional ischemia. Patients are asymptomatic; no treatment required. D/C or reduce med if very long. 4 First Degree AV Block PR = 0.34s P waves can follow T wave very closely or be hidden 5 Second Degree AV Blocks Mobitz Type I (Wenckebach) PR interval lengthens with each successive beat. This is due to gradually deteriorating conduction through the AV node until an impulse is dropped; the AV node then recovers and the cycle repeats itself. PR may become very prolonged Caused by meds, degeneration of AV node, ischemia-especially inferior MI (RCA usually supplies AV node) 6 Type I 2nd degree AV block Note the progressively longer PR interval until a QRS is dropped. The rhythm is irregular because of the dropped QRS. It is often regularly irregular 7 Type I 2nd degree AV block Treatment Usually none; patients are mostly asymptomatic. Reduce or D/C meds that may contribute if QRS is frequently dropped. If high grade, a pacemaker may be needed. 8 Type II 2nd degree AV block Block occurs below the AV node Random drop of a QRS on ECG QRS is usually prolonged due to infranodal conduction system disease. May progress to 3rd degree AV block If due to ischemia, usually anterior MI (LAD). Most often requires a pacemaker, unless lower grade and heart rate is adequate. 9 Type II 2nd degree AV block QRS dropped High grade 2nd degree AV block 10 Type II 2nd degree AV block QRS is dropped after every 2 beats with a constant PR interval. QRS is somewhat wide, which is common. 11 High Grade AV Block Most likely to be type II 2nd degree AV block, but can be type I where the PR interval doesn’t have a chance to lengthen before a QRS is dropped. 12 3rd Degree (Complete) Heart Block Lack of conduction between atria and ventricles P waves should march out and be independent of QRS complexes. P waves may be hidden, so look carefully Escape beats, either junctional (rate 40-60), or ventricular (20-40) usually appear. Block may be anywhere in AV node to bundle branches; this level determines escape rhythm. 13 Escape Rhythm If block is high in AV node: junctional escape rhythm If block is low in AV node: ventricular escape rhythm 14 3rd Degree (Complete) Heart Block Notice wide, slow QRS complexes-ventricular escape rhythm 15 3rd Degree Heart Block p p p p p p p p 16 3rd Degree AV Block junctional escape rhythm (slower than usual) 17 Intraventricular Conduction Defects RBBB LBBB Fascicular blocks (part of left bundle branchwe won’t cover these). 18 BBB Changes Normally the QRS is a composite of depolarization of the ventricles. In a bundle branch block, the R waves are separated because the ventricles depolarize separately. 19 Right Bundle Branch Block Conduction proceeds across septum from left, thus axis may shift to the right QRS greater than 0.12 sec RSR’ in V1 (often V2 and V3) Wide, slurred S waves in V6 Secondary ST&T wave changes in V1-V3 Often large R’ in V1 20 RBBB 21 RBBB 22 RBBB Occasionally more extensive ST-T wave changes 23 RBBB R-R’ are closer together 24 RBBB cont. Causes: Occasional normal finding Almost any right sided heart disease, pulmonary hypertension, PE, etc. Usually not ischemic Imitators: RVH, posterior MI, WPW(Large R in V1) Treatment: none 25 LBBB Depolarization proceeds from right to left Therefore axis may shift left Septal depolarization is lost (no Q in I, aVL,V5-6) Broad, deep monophasic QS complex in V1 and wide, notched R in 1 and V6 Widespread T wave and QRS changes make diagnosing ischemia/infarct difficult. QRS voltages can imitate LVH so usual criteria not used. 26 LBBB 27 LBBB 28 LBBB 29 LBBB 30 LBBB Causes are multiple: degenerative, HTN, acute MI, valvular anomalies. Not seen in normal hearts. BBBs may be intermittent or rate related-as heart rate speeds up, QRS can widen out. 31 CHAMBER ENLARGEMENT 32 Atrial Overload “Overload” is a better term because ECG changes may be seen with increased volume and pressure, not exclusively with atrial hypertrophy. Atrial “enlargement, hypertrophy, or abnormality” are terms often used. 33 Right Atrial Overload ECG Features Tall, peaked p waves in lead II > 2.5 mm high Biphasic p wave in V1 with a tall, initial deflection. Causes include pulmonary hypertension, RV infarct, any right sided valvular abnormality, many left sided valvular abnormalities 34 RAO 35 Notice the markedly tall and peaked P waves in leads I and II; the P wave in V1 is also large. 36 Left Atrial Overload Wide, notched p wave in I or II at least 0.12 seconds long (3 small boxes) Biphasic p wave in V1 that is at least 1 mm deep and 0.04 seconds in duration. Note that a biphasic p in V1 is normal if each component is no larger than 1mm x 1mm. Causes: Mitral valve disease, LVH, HTN, aortic valve disease, cardiomyopathy 37 69 y/o with hypertension and mitral regurgitation Large terminal component in V1 AND Wide and notched P wave in II Indicate LAO 38 Atrial Overload Patterns 39 Atrial Overload Only need criteria in lead II or V1 to diagnose atrial overload. Both are not required 40 Ventricular Hypertrophy 41 Right Ventricular Hypertrophy Initially, right axis deviation may be the only finding-this occurs because the RV mass begins to overshadow the left. Classic changes occur when hypertrophy is advanced 42 ECG changes in RVH: Reversal of normal precordial QRS pattern with a tall R wave in V1 & V2 and deep S waves in I, aVL, V5, V6. 43 ECG changes in RVH: Voltage criteria include: (use any one) R > S in V1 R in V1 at least 7 mm R in V1 + S in V6 at least 11 mm 44 RVH Repolarization change or strain pattern in the right precordial leads (V1-V3). 45 Elderly man with pulmonary HTN Right Axis Deviation Large R in V1 with associated repolarization changes. 46 62 y/o with dyspnea 47 Left Ventricular Hypertrophy Several scoring systems have been developed throughout the years, each with it’s own sensitivity and specificity. One of the more commonly used is the RomhiltEstes system. The Cornell Criteria are also sometimes used. 48 LVH Scoring 49 LVH Criteria: Voltage (need only one) R in V5 or V6 at least 30 mm S in V1 or V2 at least 30 mm R in aVL > 11 mm (most specific sign) S in V1(or V2?) + R in V5 or V6 > 35 mm R in I > 15 mm (some say 20 mm) 50 To Diagnose LVH: Combine voltage with: Strain pattern in lateral leads or Left Atrial Overload or Left Axis Deviation 51 66 y/o with long hx of HTN 52 Voltage*-3 pts Left Axis Dev.-2 pts Repolarization-3 pts LAO-2 pts 53 Unknown 54 Voltage Criteria for LVH but no other criteria 55