How to Read an EKG
advertisement

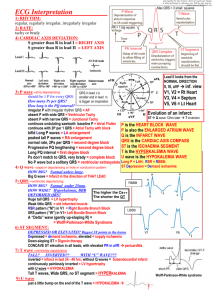
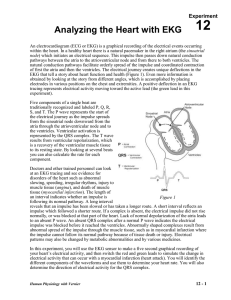
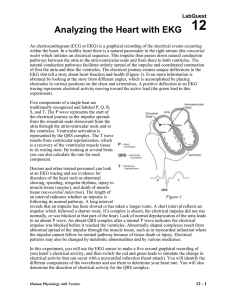
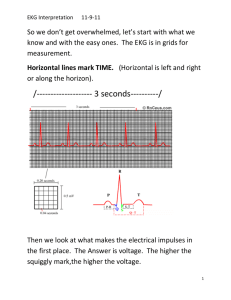
How to Read an EKG Jason Ryan, MD Intern Report How to read an EKG 1. Rate and Rhythm how fast/slow regular/irregular wide/narrow 2. Axis and Intervals PR, QRS, QT 3. Hypertrophy LAE/RAE LVH/RVH 4. ST Changes and Q waves How to read an EKG Rate 40 300 100 60 150 75 50 (-) How to read an EKG -90o Lead aVF (+) Axis QRS LAD Lead I (-) -180o (+) 0o RAD Normal Axis 90o How to read an EKG Intervals Correct QT 1. QTc=QT/(RR)1/2 (Bazett) 2. QTC=QT + 0.00175(HR60) (Hodges) PR 0.14-0.21 QRS 0.7-011 QTc <0.46 How to Read and EKG Atrial Enlargement How to Read and EKG Ventricular Enlargement Sinus Rhythm Rate between 60 to 100 P wave before every QRS – Smooth contour – Either all positive or all negative except V1 – <0.12s and <0.2mv Upright P waves in I, II, aVF Negative P wave in aVR Limb Lead Reversal Right and Left arm reversed – P wave positive aVR – P wave negative aVL and I – Limb leads look normal Right arm and Right leg reversed – P wave positive aVR – P wave negative I, L – Lead II isoelectric (almost no QRS) Left Bundle Branch Block Criteria: – QRS > 120ms (3 small boxes) – Broad, notched, or slurred R waves in I, aVL, and V5V6 – Secondary ST-T changes in I, aVL, and V5-V6 – Absence of Q waves in I, V5-V6 – R-wave peak time >60ms (1.5 small boxes) V5-V6 Separate criteria for STE AMI Right Bundle Branch Block Criteria: – QRS >120ms (3 small boxes) – R’ in the right precordial leads with R’>R – Secondary ST-T changes in R precordial leads Supporting findings: – Slurred S wave in I, aVL, left precordial leads Usual criteria for STE AMI apply Left Ventricular Hypertrophy SV1orV2+ RV5orV6>35mm – >40 if 30-40yrs old – >60 if 16-30yrs old RaVL>11mm RI + SIII >25mm RaVL + SV3 >28mm(men) or 20mm(wmn) Left Ventricular Hypertrophy Associated ST-T wave abnormalities – STD and TWI in V5-V6 Leads where QRS is mainly positive – Slight STE with upright T in V1-V2 Leas where QRS is mainly negative Sinus Tachycardia All sinus rhythm criteria – P before every QRS – Upright P in I, II, aVF – Inverted P aVR Rate >100 T Wave Inversions Indicative of subendocardial or evolving ischemia Can be a normal variant in several leads or in the presence of BBB Can be caused by several other conditions – Hypertrophic obstructive cardiomyopathy – Intracranial processes (hemorrhage) – Medications or electrolyte abnormalities – Myocarditis/pericarditis or pulmonary embolism ST depressions Horizontal ST depressions are strongly suggestive of ischemia in the appropriate clinical setting Don’t necessarily localize – Stress testing – Reciprocal changes Several other conditions can provoke ST depressions: – LVH – Medications or electrolytes – Bundle Branch Block – Pulmonary embolism ST Elevations Localizes best of all ischemic EKG changes Usually indication of acute myocardial injury (occluded artery) Several conditions can also cause ST elevations: – – – – Pericarditis Early repolarization LBBB LVH ST Elevation MI Evolution of EKG changes Normal Acute Hours 1-2 Days 3-7 Days > 7 Days Leads go together Anterior Leads go together Lateral Leads go together Inferior