VAQ ANSWER GUIDE

VAQ ANSWER GUIDE
VAQ 1
The single slice of this axial CT pulmonary angiogram post contrast administration shows a moderately large thrombus sitting at the bifurcation of the two pulmonary arteries – Saddle
Embolus.
The marking breakdown is 4 marks for the part (a) and 6 marks for part (b). This reflects that there is only limited information in the image and it should be the lesser of the two halves.
In part (b) candidates should reflect on the different treatment options including, anticoagulation, subcutaneous clexane, oral warfarin, IV heparin. The option of thrombolysis and its relative indications/contraindications to its use. My thought being that limb surgery being lower risk of significant bleeding than truncal or cerebral surgery.
Surgical embolectomy - +/-transfer to a cardiothoracic unit.
VAQ 2
A broad, bizarre QRS complex tachycardia should only mean hyperkalaemia and +/- possibly severe toxidrome leading to the hyperkalaemia.
Immediate treatment of hyperkalaemia should include the hierarchy of medications used including insulin (+dextrose), β 2 agaonist, calcium, bicarbonate, resonium.
Further management dictated by response to medical therapy, acid-base balance and evidence of cardiac or renal failure leading to dialysis.
VAQ3
SEVERE METABOLIC ALKALOSIS – CHLORIDE RESPONSIVE
His respiratory and neurologic systems were unremarkable. The abdomen was distended and multiple fluid and air levels seen on an abdominal radiogram, confirmed sub acute intestinal obstruction.
Despite denials of use of any diuretics or laxatives, when his regular medicines were checked, loop diuretics and combinations with potassium sparing diuretics were recovered-confirming long term diuretic abuse. All diuretics were removed from patient's bedside and patient was hydrated to achieve a central venous pressure (CVP) of at least 10 cm water (opening CVP 1 cm water) and a urine output of more than 1 ml/kg/hour. Obstipation was relieved by manual evacuation of hard dried up faeces - the cause of sub acute intestinal obstruction.
Supplementation of potassium, chloride, sodium and magnesium led to improvement of serum electrolytes and resolution of alkalemia over 36 hours. The patient's respiratory distress, weakness and lassitude resolved. Patient was discharged after four days without any complains.
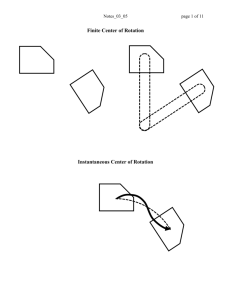
VAQ4
ATRIAL TACHYCARDIA WITH SECOND DEGREE AV BLOCK TYPE 1 (WENCKEBACH, MOBITZ 1) AND
3:2 CONDUCTION, VENTRICULAR RATE 115, INCOMPLETE RBBB.
This rhythm was initially misdiagnosed at atrial fibrillation because of its irregularity.
However close inspection reveals that the rhythm is actually regularly irregular. Regular irregularity of the cardiac rhythm, whether in the setting of a bradycardia or a tachycardia, should prompt consideration of a second degree AV block. Lead V1 reveals distinct atrial activity at a rate of 172. A 3:2 atrial:ventricular contraction ratio occurs; prolongation of the PR-interval is noted
from the first P-QRS complex to the next, then the third atrial contraction is non-conducted and followed by a pause before the cycle repeats. Although second dehgree AV block usually occurs in conjunction with bradydysrhythmias, Mobitz 1 also occasionally occurs in the presence of tachydysrhythmias, a fact that is not well known. As a result, these rhythms are often misdiagnosed as rapid atrial fibrillation. Recognizing that these rhythms are regularly irregular provides a major clue to the proper diagnosis.
(ECG and text taken from – ECGs for the Emergency Physician 2 – Amal Mattu and William Brady;
Blackwell Publishing)
VAQ 5
A dislocated ankle to the fibula side with tight overlying skin, pale and shiny; dusky skin around it thereby it should be stated that there is skin viability circulatory issues. The overlying wound whilst unlikely to communicate with the bone, suggests more deep abrasion than open dislocation.
Distal foot perfusion also compromised.
Management should address the need for reduction and to be performed prior to imaging although immediate bedside imaging may be utilized whilst getting ready for analgesia and sedation, reduction and plastering. Answers should address the medications and doses to be used and noting the allergy to eggs precludes propofol
VAQ 6
A huge quantity of information for candidates to work through but should prove to be able to discriminate the better candidates from the weak ones. Basically a case of Hyperosmolar diabetic coma. Correction of the sodium for the glucose would put it around normal or just high depending on what formula is used. Significant pre-renal renal impairment probably secondary to volume depletion. A severe raised anion gap acidosis without significant respiratory compensation.
Question is whether to use the corrected sodium value for calculation of your anion gap.
The CK probably reflects a prolonged lie but also need to differentiate if a cardiac event occurred by
CKMB or troponin tests. The initial cause of the collapse may have been cardiac.
A great set of numbers!
VAQ 7
SINUS RHYTHM WITH FIRST DEGREE AV BLOCK, RATE 93, LBBB, ST-SEGMENT ABNORMALITY
CONSISTENT WITH ACUTE ISCHAEMIA OR AMI
In this case concordant ST segment elevation >1mm is present in lateral leads I, aVL, V5 and V6 consistent with acute MI. Excessive discordant ST segment elevation >5mm is also present in leads
V1-V4.
LBBB is associated with characteristic repolarization abnormalities. In all leads, ST –segments are displaced in an opposite direction to the terminal deflection of the QRS complex. The magnitude of this “discordance” is allowed to be up to 5mm.
In 1996 Sgarbossa published a set of criteria that utilize this expected ST-segment discordance to make predictions about the chances of a patient with LBBB having an AMI. She stated that acute MI should be strongly considered in the presence of LBBB when any of the following apply: (1) ST segment elevation >1mm is concordant (in the same direction) with the QRS complex; (2) STsegment depression of >1mm is present in leads V1, V2 or V3 (i.e concordant ST-segment depression in these leads); or (3) ST-segment elevation of >5mm is discordant with the QRS complex. Although the sensitivity of any of these findings is low, the specificity (likelihood of ruling in for AMI) is extremely high, and the presence of any of these “Sgarbossa criteria” is now considered reasonable justification to provide immediate fibrinolytics or PCI to patients with LBBB and angina symptoms (the presence of a new LBBB is also sufficient criteria to initiate these measures).
(ECG and text taken from – ECGs for the Emergency Physician 2 – Amal Mattu and William Brady;
Blackwell Publishing)
VAQ 8
The right-sided pneumothorax should be obvious to all but the left sided one is more subtle. I suspect a lot of candidates will miss the left sided pneumothorax having seen “major pathology on the opposite side”. No rib fractures are seen and no subcutaneous emphysema. Important negatives also include the absence of mediastinal shift, tracheal deviation etc. Conservative management of either pneumothoraces if contemplated should recognize complications, implications and expected duration of recovery.
Candidates should give an estimation of size and give a sound rationale for the management they propose. Better candidates should relate the answer back to the question in relation to his employment as a military pilot. Although this is traumatic rather than spontaneous, a correlation of the injury and his ability to fly should be made.
This x-ray is a good one to make them look closely at all aspects of the film and not just at what first catches the eye.
Management should include the decision to aspirate, drain; via small caliber or larger drain, bilateral drains.
Supportive care to include analgesia and disposition to also relate to the stem of his occupation and the importance of specialist follow up and decision on ongoing flying etc.