coma
advertisement

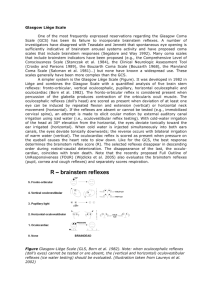
Alerted conscious (coma) What is consciousness? Consciousness is a state of wakefulness and awareness of self and surroundings. What is coma? Coma is a state of altered consciousness with loss of both wakefulness (arousal, vigilance) and awareness. Consciousness means you see, talk, interact with environment ,so ,it is controlled by many centers in cerebral cortex(both),so to loss this Consciousness you must had bilateral cerebral cortex affection . Cerebral cortex to work need activation from reticular activating system in brain stem. So to had coma lesion may be A)diffuse cerebral cortex lesion(bilateral),or B)brain stem injury. Trauma Parenchymal injury Intracranial hemorrhage Epidural hematoma Subdural hematoma Subarachnoid hemorrhage Intracerebral hematoma Diffuse axonal injury Nontraumatic causes Toxic/metabolic Hypoxic-ischemic encephalopathy Shock Cardiopulmonary arrest Near-drowning Carbon monoxide poisoning Toxins Medications: narcotics, sedatives, antiepileptics, antidepressants, analgesics, aspirin Environmental toxins: organophosphates, heavy metals, cyanide, mushroom poisoning Illicite substances: alcohol, heroin, amphetamines, cocaine Systemic metabolic disorders Substrate deficiencies Hypoglycemia Cofactors: thiamine, niacin, pyridoxine Electrolyte and acid-base imbalance: sodium, magnesium, calcium Diabetic ketoacidosis Thyroid/adrenal/other endocrine disorders Uremic coma Hepatic coma Reye syndrome Inborn errors of metabolism Urea cycle disorders Amino acidopathies Organic acidopathies Mitochondrial disorders Infections/postinfectious/inflammatory Meningitis and encephalitis: Bacterial, viral, rickettsial, fungal Acute demyelinating diseases Acute disseminated encephalomyelitis Multiple sclerosis Inflammatory/autoimmune Sarcoidosis Sjögren disease Lupus cerebritis Mass lesions Neoplasms Abscess, granuloma Hydrocephalus Paroxysmal neurologic disorders Seizures/SE Acute confusional migraine Vascular Intracranial hemorrhage Arterial infarcts Venous sinus thromboses 1)superatentorial as hage,tumor,hematoma Or metabolic,hypoxic-ischeamic,infection 2)infratentorial hage,embolic,thrombetic,tumor Skull is closed box. So you need to know A)there is increase in I.C.P. B)there is herniation syndromes or not. C)there is convulsion or not. Increase I.C.P. present in almost all comatosed patient ,due to associated brain oedema. It may be mild undetected or may be sever life therating. 1)bulging anterior fontanel 2)neurologically: -sluggish pupillary reaction -increase tone -hyper-reflexia -hyperventilation with deep inspiration and expiration. 3)Cushing respose:late,not constantly present (hypertension,bradycardia,abnormal respiration),=impending herniation Herniation syndromes 1)Central herniation Increased pressure in both cerebral hemispheres, causing downward displacement of the diencephalon through the tentorium, causing brainstem compression. Diencephalic stage: withdraws to noxious stimuli, increased rigidity, or decorticate posturing; small, reactive pupils with preserved oculocephalic and oculovestibular reflexes; yawns, sighs, or Cheyne-Stokes breathing. Midbrain-upper pons stage: decerebrate posturing or no movement; mid-position pupils that may become irregular and unreactive; abnormal or absent oculocephalic and oculovestibular reflexes; hyperventilation. Lower pons-medullary stage: no spontaneous motor activity, but lower extremities may withdraw to plantar stimulation; mid-position fixed pupils; absent oculocephalic and oculovestibular reflexes; ataxic respirations. Medullary stage: generalized flaccidity; absent pupillary reflexes and ocular movements; slow irregular respirations, death. 2)Uncal herniation Uncus of the temporal lobe is displaced medially over the free edge of the tentorium. Ipsilateral third-nerve palsy (ptosis, pupil fixed and dilated, eye deviated down and out). Ipsilateral hemiparesis from compression of the contralateral cerebral peduncle (Kernohan notch). Other signs of brainstem dysfunction from ischemia secondary to compression of posterior cerebral artery. 3)Subfalcine (Cingulate) herniation Increased pressure in one cerebral hemisphere leads to herniation of cingulated gyrus underneath falx cerebri. Compression of anterior cerebral artery leads to paraparesis. 4)Tonsillar herniation Increased pressure in the posterior fossa leads to brainstem compression. Loss of consciousness from compression of reticular activating system. Focal lower cranial nerve dysfunction. Respiratory and cardiovascular function can be significantly affected early with relative preservation of upper brainstem function, such as pupillary light reflexes and vertical eye movements. 1)history 2)general examination 3)neurological examination a)level of consciosness b)respiratory pattern c)motor response d)eye examination 1)level of consciousness a-depressed consc. lethergy:conscious but look sleepy confusion:conscious but with disorientation of the surroundings b)unconsciousness(coma):4 stages -stupor:can be aroused briefly(less than one minute)then become uncosciosness --light coma can not be aroused,respond by motor ---Deep coma no respose to painful stemuli ----Deep coma with apenea. Comatose patients with metabolic disease – Confusion, stupor and coma precede motor signs – The motor signs are usually symmetrical – The EEG is generally very slow – Caloric stimulation elicits either tonic deviation of the eyes or, if the patient is deeply comatose, no response – Seizures are common Abnormal focal motor signs (including focal seizures) occur, which progress rostrally to caudally, and are asymmetrical – Neurological signs :point to one anatomical area (mesencephalon, pons, medulla) – Specific cognitive function disorders, such as aphasia, acalculia, or agnosia, appear out of proportion to a general overall decrease in mental state – The EEG may be slow, but in addition there is a focal abnormality When present urgent C.T.and neurosurgical consultation is life –saving. 1)asymmetric motor response 2)asymmetric brainstem reflexes. 3)uncal herniation. 4)focal convulsion Table 53.2 Initial evaluation of coma Airway, breathing, and circulation assessment and stabilization Ensure adequate ventilation and oxygenation. Blood pressure management depends on considerations regarding underlying coma etiology. If hypertensive encephalopathy or intracranial hemorrhage, lower blood pressure. If perfusion-dependent state, such as some strokes or elevated intracranial pressure, reducing blood pressure may reduce cerebral perfusion. Draw blood for glucose, electrolytes, ammonia, arterial blood gas, liver and renal function tests, complete blood count, lactate, pyruvate, and toxicology screen. Neurologic assessment GCS score Assess for evidence of raised intracranial pressure and herniation. Assess for abnormalities that suggest focal neurologic disease. Assess for history or signs of seizures. Administer glucose IV (in an adult, thiamine should be given first) If concern for infection delays lumbar puncture, broad-spectrum infection coverage should be provided (including bacterial, viral, and possibly fungal). Give specific antidotes if toxic exposures are known. For opiate overdose, administer naloxone. For benzodiazepine overdose, consider administering flumazenil. For anticholinergic overdose, consider administering physostigmine. Identify and treat critical elevations in intracranial pressure. Neutral head position, elevated head by 20 degrees, sedation. Hyperosmolar therapy with mannitol 0.25–1 g/kg or hypertonic saline. Hyperventilation as temporary measure. Consider intracranial monitoring. Consider neurosurgical intervention. Head CT (non-contrast) Treat seizures with IV anticonvulsants. Consider prophylactic anticonvulsants. Investigate source of fever and use antipyretics and/or cooling devices to reduce cerebral metabolic demands. Detailed history and examination Consider lumbar puncture, EEG or extended video EEG monitoring, MRI, metabolic testing (amino acids, organic acids, acylcarnitine profile), autoimmune testing (ANA panel, antithyroid antibodies), thyroid testing (TSH, T3, T4). Skull is closed box so it is easy to develop, 1)increase I.C.P. 2)herniation syndroms 3)seizures Subclinical seizures in critically ill patients may be an under-recognized phenomenon; therefore, the index of suspicion in a comatosed child shoud be high. recent study of nonresponsive children in an ICU demonstrated that 33% of children manifested electrographic patterns consistent with nonconvulsive status epilepticus (NCSE). Delayed diagnosis associated with high mortality.