Altered Mental Status

Pediatric Neurology Quick Talks
Altered Mental Status
Michael Babcock
Summer 2013
Scenario
• 8yo boy
• Found stumbling around garage about 30 minutes ago
•
Asleep on arrival, arouses to sternal rub
•
Has 30 second GTC in ED bay.
•
Pupils reactive b/l, oculocephalics intact
•
Increased tone on R and upgoing R toe.
Altered Mental States
• Agitation – not a normal state
• Delirium ( Latin – to go out of the furrow ) – more floridly abnormal mental state, misperception of sensory stimuli, visual hallucinations.
• Lethargy – Clouding of consciousness – reduced awareness
• Obtundation ( Latin – to beat against or blunt ) – mild/moderate reduction in alertness.
•
Stupor ( Latin – to be stunned ) – deep sleep/unresponsiveness from which patient can be arouse only with vigorous/continuous stimulation.
•
Coma ( Latin – deep sleep or trance ) – state of unresponsiveness in which patient lies with eyes closed and cannot be aroused even with vigorous stimulation.
•
Really, better to just DESCRIBE state.
After coma – Other prolonged states
• Coma is transient – patients recover, die, or evolve
• Minimally conscious state – severely impaired consciousness in which minimal, but definite, behavioral evidence of self or environmental awareness is demonstrated
•
Vegetative state
– recovery of crude cycling of arousal states – “eyeopen” periods in unresponsive patient. Few surviving patients with forebrain damage remain in eyes-closed coma for more than 10-30 days.
•
Brain death
– irreversible loss of all functions of the entire brain.
Not Coma
• Paralysis
– Locked-in state – voluntary vertical eye movements, blinking.
– Severe peripheral nerve paralysis – GBS, botulism
•
Akinetic-mutism / abulia
– Frontal lobe lesions
– Pt doesn't move or speak
– Retains awareness – often tracks
– Exam normal, oculocephalics normal
• Psychiatric unresponsiveness / catatonia
– Maintain trunk/limb postures
– Exam changes unpredictably
– Resist passive eye opening
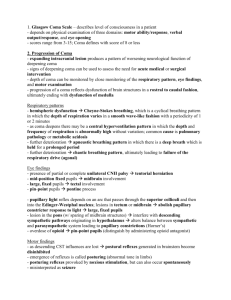
Causes of Coma
• To cause coma state, must either:
– 1. produce bilateral dysfunction of cerebral hemispheres
– 2. damage/depress physiologic activating mechanisms
• Lie along central core of upper brainstem and diencephalon
– 3. metabolically or physiologically damage or depress brain globally
Differential conditions – 4 types
• 1. Supratentorial mass lesions
– compress/displace brainstem/diencephalon
– Signs of focal cerebral dysfunction present at onset
– Signs of dysfunction progress rostral to caudal
– Neurologic signs point to one anatomic area
– Motor signs often asymmetric
• 2. Infratentorial mass lesions
– destructive/expanding lesions damage/compress reticular formation
– History of preceding brainstem dysfunction OR sudden onset of coma
– Localizing brainstem signs precede/accompany onset of coma
– Abnormal pupillary/oculomotor findings usually present
Differential Conditions – 4 types
• 3. Metabolic/diffuse/multifocal
– confusion/stupor commonly precede motor signs
– Motor signs usually symmetric
• Though CAN be asymmetric!
– Pupillary reactions usually preserved
– Asterixis / myoclonus
– Tremor / seizures
– Acid-base imbalance with hyper/hypo-ventilation
•
4. Psychiatric
– Lids actively closed
– Pupils reactive or medically dilated (cycloplegics)
– Oculocephalic responses are unpredictable
• Oculovestibular responsephysiologic wakefullness
– Motor tone is inconsistent or normal
– Normal or hyperventilation
– No pathologic reflexes
– EEG normal
History
• Onset – abrupt or gradual
• Recent complaints
– HA
– Depression
– Focal weakness
– Vertigo
•
Recent injury / trauma
•
Previous medical illness
• Previous psychiatric illness
Coma Examination
• Vitals
• Assess level of consciousness
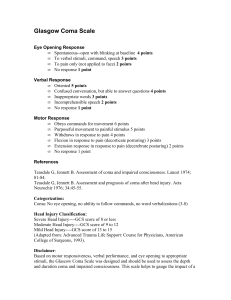
– Glasgow coma scale – quick; developed for head trauma
•
Pattern of breathing
•
Size/reactivity of pupils
– Fundoscopic examination
•
Eye movements and oculovestibular response
•
Brainstem reflexes
• Skeletal motor responses
– spontaneous/withdrawal/patterned
– DTR's
– babinski
Cushing's Triad
• Sign of Increased ICP
• Increased BP (widened pulse pressure)
•
Bradycardia
•
Irregular respirations
Work-up
• Vitals
• Venous blood
– Glucose
– Electrolytes, BUN/ Cr
– CBC
– Coags
– LFTs, ammonia
– TFTs
– Blood cultures
– Viral titers
– Tylenol / asa
• Arterial blood
– pH, pO2, pCO2
– carboxyhemoglobin
•
? CSF
– Cells
– Gram stain
– Glucose / protein
– cultures
• Other tests
– Urine culture / UDS
– EKG
– Head CT
– Consider EEG
Brain Death
•
Known irreversible cause (rule out reversible causes)
•
Normothermic (>35 deg C), normotensive, metabolic disturbances corrected
•
Coma + apnea + loss of all brain stem reflexes + absent spontaneous/induced movements (beside spinal reflexes)
•
Sedative, analgesics, NM blockers, (anti-convulsants), discontinued for reasonable time, can use plasma levels to check
•
Two exams with observational period.
•
Observation period – 24 hours if < 1 month; 12 hours if > 1 month.
•
Ancillary studies including EEG and Cerebral blood flow not required, and are not substitute for exam
–
Useful when components of exam or apnea testing cannot be safely completed, uncertainty about examination, medication effect may interfere, need to reduce observation period.
•
EEG – Electrocerebral silence – no EEG activity over 2 uV.
References
1. Posner, Jerome; Spaer, Clifford; Schiff, Nicholas; Plum, Fred. 2007. Plum and Posner's Diagnosis of Stupor and
Coma.. 4 th ed. New York: Oxford Press.
2. Nakagawa TA, Ashwal S, Mathur M, Mysore MR, Bruce D, Conway EE Jr, Duthie SE, Hamrick S, Harrison R,
Kline AM, Lebovitz DJ, Madden MA, Montgomery VL, Perlman JM, Rollins N, Shemie SD, Vohra A,
Williams-Phillips JA, Society of Critical Care Medicine, Section on Critical Care and Section on Neurology of the American Academy of Pediatrics, Child Neurology Society. Guidelines for the determination of brain death in infants and children: an update of the 1987 Task Force recommendations. Crit Care Med. 2011
Sep;39(9):2139-55. [91 references]