Unlocking the secrets of
locked-in syndrome
By Rachel L. Palmieri, RN-C, ANP, MS
Nursing2009, July 2009
2.4 ANCC contact hours
Online: www.nursingcenter.com
© 2009 by Lippincott Williams & Wilkins. All world rights reserved.
Locked-in syndrome (LIS)
Complete paralysis of voluntary
muscles in all parts of the body
except those that control blinking
and vertical eye movements
Patients with the classic form are
conscious and can think and reason
but can’t speak or move anything
except their eyes
Causes
Rare neurologic disorder
Caused by primary vascular or
traumatic brainstem injury
Usually a ventral pons lesion from
injury or obstruction of basilar artery
Traumatic brain injury can be a result
of direct brainstem contusion or
vertebrobasilar axis dissection
Other causes of LIS
Brain tumors that invade ventral pons
Prolonged hypoglycemia
Damaged nerve cells, especially
myelin sheath (such as in MS)
Hemorrhage in pons
Ischemia
Overdose
End stages of ALS
LIS signs and
symptoms/characteristics
Preserved
consciousness
with upper
motor neuron
quadriplegia
Paresis
Hyperreflexia
Clonus
Initial
contralateral
flaccid paralysis
Paralysis of cranial
nerves VII, IX, X,
XII produces
facial, tongue,
pharynx paralysis
Severe difficulties
in swallowing and
speech
LIS characteristics
Sensation remains intact
Temporary LIS can be
pharmacologically induced
Prognosis is unpredictable
Early aggressive treatment promotes
best outcomes
Incidence of LIS
Difficult to detect; often misdiagnosed
as coma, persistent vegetative state,
or minimally conscious state
367 patients from 1997-2004 have
been registered by the Association du
Locked-In Syndrome based in France
Neurologists believe many more cases
are undetected
Categorizing LIS
Classified into three categories:
- classic: quadriplegia, with eye
movement
- incomplete: remnants of voluntary
movement (arm, hand, face)
- total: total immobility, conscious,
inability to communicate
Diagnosis
Key is assessing for voluntary vertical
eye movement
MRI is preferred method for detecting
pons lesions
Neurologist should reexaimne patient
once a lesion is confirmed
Diagnosis
EP (evoked potential) testing can
provide information about brain
function
EEG is controversial
Definitive diagnosis can take months
to years; family/healthcare providers
must observe patient closely
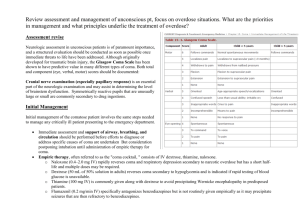
Assessment tools
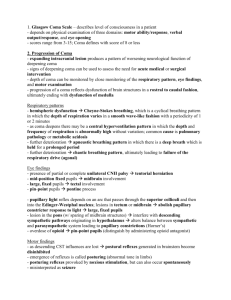
Glasgow Coma Scale (GCS) used
to be gold standard
Full Outline of Unresponsiveness
(FOUR) score developed in 2005 at
Mayo Clinic supplements GCS
FOUR Score Coma Scale
FOUR Score Coma Scale includes four
subscales to score separately for eye
response, motor response, brainstem
reflexes, respiration
Lower scores indicate more severe
signs and symptoms
FOUR Score Coma Scale
Eye response (E)
Try to elicit best level of alertness by
using at least 3 trials, then grading
best response
If patient’s eyes are closed, open them
and see if patient tracks a finger or
object
FOUR Score Coma Scale
In cases of eyelid edema or facial
trauma, tracking with only one open
eyelid will suffice
If horizontal tracking is absent,
examine patient for vertical tracking
Alternatively, document 2 blinks on
command, which indicates LIS
(patient is fully aware)
FOUR Score Coma Scale
E4:Eyelids open or opened, tracking,
or blinking to command
E3: Eyelids open but not tracking
E2: Eyelids closed, open to loud
voice, not tracking
E1: Eyelids closed, open to pain, not
tracking
E0: Eyelids remain closed with pain
FOUR Score Coma Scale
Motor response (M)
Grade best possible response of arms
If patient demonstrates at least 1 of
3 hand positions with either hand,
score is M4
FOUR Score Coma Scale
If patient touches or nearly touches
examiner’s hand after painful
stimulus compressing the
temporomandibular joint or
supraorbital nerve, score is M3
If patient has any flexion movement
of the upper limbs, including
withdrawal or decorticate posturing,
score is M2
FOUR Score Coma Scale
M4: Thumbs up, fist, or peace sign to
command
M3: Localizing to pain
M2: Flexion response to pain
M1: Extensor posturing
M0: No response to pain or
generalized myoclonus status
epilepticus
FOUR Score Coma Scale
Brainstem reflexes (B)
Examine pupillary and corneal reflexes
Preferably, test corneal reflexes by
instilling few drops of saline on cornea
from distance of several inches to
minimize corneal trauma from
repeated exams, or use cotton swabs
FOUR Score Coma Scale
Test cough reflex to tracheal
suctioning only when both reflexes
are absent
Score of B1 indicates both pupil and
corneal reflexes are absent but cough
reflex (using tracheal suctioning) is
present
FOUR Score Coma Scale
B4: Pupil and corneal reflexes
present
B3: One pupil wide and fixed
B2: Pupil or corneal reflexes absent
B1: Pupil and corneal reflexes
absent
B0: Absent pupil, corneal, and
cough reflex
FOUR Score Coma Scale
Respiration (R)
For ventilated patients, use
respiratory patterns shown on
ventilator monitor to identify patientgenerated breaths
Don’t adjust ventilator while patient is
graded; try to ensure patient has a
PaCO2 within normal limits
FOUR Score Coma Scale
To assess breathing drive, may need
to disconnect ventilator for 1-2
minutes while providing oxygenation
Standard apnea test may be needed
when patient is breathing at
ventilator rate
FOUR Score Coma Scale
R4: Not intubated, regular
breathing pattern
R3: Not intubated, Cheyne-Stokes
breathing pattern
R2: Not intubated, irregular
breathing pattern
R1: Breathes above ventilator rate
R0: Breathes at ventilator rate or
apnea
Finding a way to communicate
Establish a blinking pattern for
communication
Establish good rapport with patient
Give patient control over care
Validate patient’s fear, anxiety, pain
Finding a way to communicate
Involve patient’s family
Educate hospital staff
Work with speech therapist
Point board system or Morse code
may be used to expand patient
communication
Nursing care
Family education regarding patient’s
care is one of the biggest needs
Stimulating the mind of the patient
with music, being read to, etc.
Coordinating interdisciplinary team
regarding patient’s care
Following a plan for patient care
Respiratory function
Place patient in lateral recumbent
position, keeping neck in neutral
position
Elevate head of bed 30 degrees
unless contraindicated
Oxygenate with 100% oxygen before
and after suctioning
Following a plan for patient care
Suction oropharyngeal airway or via
endotracheal/tracheostomy tube
every 1-2 hours to clear drainage.
Limit suctioning to 10 seconds or less,
1 insertion per attempt
Provide tracheostomy care every 4
hours
Frequently monitor rate, depth,
pattern of respirations
Following a plan for patient care
Observe frequently for signs and
symptoms of respiratory distress
Auscultate chest every 2 hours for
adventitious sounds
Monitor ABG values periodically,
continue pulse oximetry
Administer supplemental oxygen as
ordered
Following a plan for patient care
Provide mouth care every 2-4 hours,
brush patient’s teeth every 8 hours
If patient is mechanically ventilated,
provide “sedation vacation” with
spontaneous breathing trial as ordered
Institute VTE prophylaxis as ordered
Following a plan for patient care
Cardiovascular function
Monitor vital signs frequently
Monitor rate, rhythm, quality of
apical and peripheral pulses
Document any dysrhythmias
Following a plan for patient care
Don’t use foot gatch under patient’s
knees or place constricting objects
behind knees
Position patient so each joint is
higher than previous joint; distal
joints will be highest
Following a plan for patient care
Integumentary system
Use lubricants, protective dressings,
proper lifting techniques to avoid skin
injury from friction/shear when
transferring/turning patient
Use pillows or other devices to keep
bony prominences from direct
contact with each other
Following a plan for patient care
Optimize nutrition and hydration
Conduct pressure ulcer admission
assessment, reassess risk daily;
inspect skin daily
Provide pressure-relieving devices
but not donut-type devices
Use protective barriers on fragile or
irritated skin
Following a plan for patient care
Don’t massage bony prominences
Perform risk assessment with a
reliable, standardized tool (Braden
Scale)
Clean skin at time of soiling; avoid
hot water and irritating cleaning
agents; use moisturizers on dry skin
Following a plan for patient care
Keep patient’s heels off bed at all
times
Turn and reposition patient at least
every 2 hours
Protect skin of incontinent patients
from exposure to moisture
Following a plan for patient care
Musculoskeletal function
Perform passive range-of-motion
exercises at least 5 times/day
Position patient in proper body
alignment, using trochanter roll,
splints, slings, pillows, etc.
Collaborate with physical therapist
Following a plan for patient care
Urologic function
Monitor intake and output
Follow strict aseptic technique in care
of patient’s urinary catheter
Remove urinary catheter as soon as
possible
Following a plan for patient care
Consider intermittent catheterization
program
Provide perineal care
Monitor urinalysis and urine culture
and sensitivity results for signs of
infection
Following a plan for patient care
Gastrointestinal function
Monitor and record character and
frequency of bowel movements
Auscultate bowel sounds
Use peptic ulcer prophylaxis as
ordered
Following a plan for patient care
Neurologic function
Provide sensory stimuli by talking to
patient; explain surroundings,
treatments
Encourage family to touch, talk to
patient
Use orientation instruments (clock,
window, favorite objects, etc.)
Following a plan for patient care
Pain
Assess for nonverbal pain indicators
Assess for distended bladder, fecal
impaction
Assess for foreign object on/under skin
Administer analgesics, provide
alternatives
Following a plan for patient care
Nutrition and hydration
Request nutritional consultation
Maintain accurate intake/output
record; include daily calorie count
Monitor skin turgor, mucous
membranes for dryness
Following a plan for patient care
Monitor urine specific gravity, serum
osmolality values
Provide hydration as ordered
Weigh patient daily
Research
Infrared eye movement sensors and
computer voice prosthetics being
developed
Tissue plasminogen activator (t-PA)
administered to patients with
evolving LIS has shown to reverse
quadriparesis when given within 3
hours