2 Main Events in
advertisement

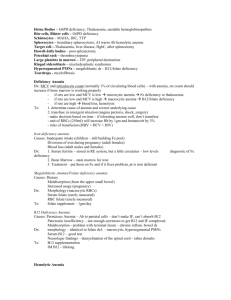
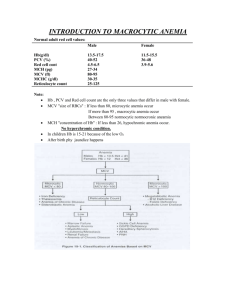
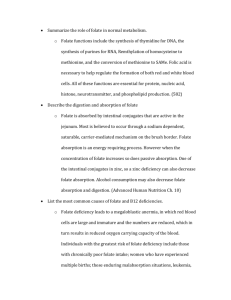
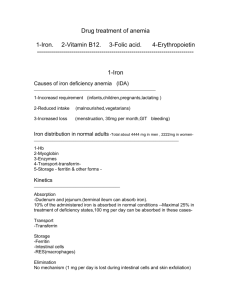
IDA develops slowly through 3 overlapping stages: 1body’s iron stores for erythrooesis are depleted 2erythropoesis begins to be affected at the same time that the hemoglobin content of the RBC’s being formed is lowered 3when small, Hb deficient RBCs enter the circulation Stages of Iron deficient anemia ! Laboratory tests to confirm IDA Microscopic Histopathology findings for IDA 1. Serum ferritin and iron concentration will be LOW (but, acute phase reactant, may go up for other reasons)Serum iron binding capacity is HIGH 2. Bone marrow—can use storage Fe, but this is painful, cumbersome 3. Treatment Hypochromia refers to lowered Hb content in RBCs (MCHC) Microcytic (MCV) These findings suggest that laboratory tests should be done to confirm IDA Signs of anemia Hematopoiesis: Stem cells Pluripotential, multipotential, progenitor, precursor Cold, pale extremitites Generalized pallor of skin and mucous membranes Jaundice (suggest hemolytic anemia) Chelosis—fissuring at the angles of the mouth (can have other causes) Koilonychia (concave nails) 0.01-0.05% of bone marrow population self-renew and differentiate pluri: self-perpetuating pool multi: can become either lymphoid or myeloid cells progen: commited to a cell lineage precursor: can prolife and develop into myeloid lineage Embryology of RBCs Bone marrow stroma 1. types of cells 2. What else? Stages of erythropoiesis? Stages of Granulopoiesis? 1. 2. 3. 4. 5. begins in fetal yolk sac shift to liver later forms in spleen term, forms in bone marrow as adult, most occurs in axial skeleton 1. fat cells, macrophages, endothelial cells, lymphocytes, and fibroblasts 2. Collagen, adhesion proteins, growth factors such as G-CSF, GM-CSF, EPO 1. proerythrobast—intense blue, round nucleus 2. basophilic erythroblast—intense blue, condensed chromatin 3. polychromatophilic erythroblast—grayish cytoplasm due to hb, smaller nuleus 4. orthochromatic erythroblast—reddish, small nucleus 5. reticulocyte—no nucleus, still has mito and RNA 6. mature erythrocyte 1. myeloblast—high N:C ratio 2. promyelocyte—primary (purple) granules 3. myelocyte—nucleus may be eccentric, cytoplasm may have pink granules 4. metamyelocytes—kidney bean shaped nucleus 5. band—horseshoe shaped nucleus 6. PMN—lobular nucleus --first line of defense for microorganisms, chemotatic, opsonins, lysosomal enzymes KNOW: hydrogen peroxide, superoxide, halides Monocytopoiesis Monoblasts mature into monocytes. Become part of mononuclear phagocyte system in tissue. Half life is 70h Chemotaxis, phagocytosis, antigen presentation, IL-1 and TNF relase (eg due to endotoxins), Megakaryocytopoiesis Eosinophils Etoposide (VP-16), teniposide (VM-26) These mature into multilobed giant cells by endomitotic divisions. Granular cytoplasm, with platelet containing ribbons Large granules stain red with eosin due to basic proteins Bilobed nucleus In tissue IgA receptors, toxic cationic proteins, kill parasites, cause allergic reactions Chemotaxis, phagocytosis, Immediate type hypersensitivity Basophils When are transfusions necessary? What are the risks? What happens? Anemia with: 1. low reticulocytes 2. normal reticulocytes 3. high reticulocytes Blue-black granules with histamine Allergic reactions Immediate type hypersensitivity Inflammatory responses Based on symptoms, NOT numbers 1. shock 2. surgery 3. angina pectoris—cornonary insufficiency, chest pain on exertion Risks: Hep B, HIV, Hep C even with testing Hb increases by 1g and hematocrit rises by 3% with 250mls. 1. marrow problem 2. ditto 3. rbc destruction or blood lossnormal marrow is accounting for decreased RBCs The low down on iron Differential diagnosis for Macrocytic anemia 3 major causes of folate deficiency How do you diagnose folate deficiency? How do you treat it? In most foods Absorbed in small intestine Transferring—carrier protein which delivers it to the marrow Ferritin—iron is stored complexed to ferritin in the liver, spleen. The body recycles iron!! Adults tend to keep their iron around 3g: 2 in erythrocytes, 1 in storage Because storage is full in adulthood, decreased iron must be due to loss of blood. 1. Folate deficiency 2. B12 deficiency Dietary (salads), Malabsorption (illium), Increased usage (pregnancy) Dx: 1. Morphology (macrocytic RBCs, hypersegmented PMNs 2. Serum folate—look for LOW levels 3. Red cell folate—look for LOW levels Treatment: 1. folate supplement, 1mg a day 3 major causes of B12 deficiency How do you diagnose B12 deficiency? How do you treat it? What is folate very important for? How long does the body store it for? Pernicious Anemia (autoimmune anti-parietal cells, therefore no IF), Malabsorption (illium), Pancreatic insufficiency (no secretion, no R/IF switch Dx: 1. Morphology (macrocytic RBCs, hypersegmented PMNs 2. Serum B12—look for LOW levels 2. Neurologic findings—demyelination of spinal cord (proprioception, cerebral cx (dementia) Treatment: B12 supplement, 1mg a day B12 is a cofactor (stored for four mo) Folic acid to dihydrofolate Without enough folate you don’t make DNA!! Folate stored for years B12 absorption Hemolytic anemias—increased RBC degradation, decreased life span of RBCs. What are clinical features? Extravascular vs. intravascular hemolytic anemai Splenomegaly Jaundice Icterus (yellow discoloration of sclerae) Ankle ulcers Aplastic crisis from Parvo B19 (infect and lyse RBCs) Pigmented gallstones composed of bilirubin Tea colored urine Increased requirement for folate 1. Extravascular: macs in spleen, liver, marrow remove damaged RBCs with Abs on them. Hemolysis occurs in cells of RE system. Little free Hb released. 2. Intravasc: destroyed directly in vasculature. Free hb released into circulation. Laboratory findings for increased RBC production Laboratory evidence for increased RBC destructoin Mech: MeatB12R factor from salivary glands binds to B12in duodenum, IF from stomach switches with R factor—pancreatic secretions are required for thisB12 is absorbed at terminal illium Elevated reticulocyte count, polychromasia Elevated MCV, RDW elevated Erythroid hyperplasia in bone marrow “frontal bossing;” marrow (skull, ribs, and long bones) expands because of increased erthropoiesis elevated LDH due to cell death elevated unconjugated bilirubin aka “indirect” bilirubin lower levels of serum haptoglobin; it binds to hb and is rapidly cleared Hemoglobinemia more hb than can be bound to haptoglobin Hemoglobinuria free hb in urine (reddish ur.) Hemosiderinuria hb in urine taken up by tubular cells and changed into hemosiderin Schistocytes, spheerocytes, bite cells or blister cells Types of congenital hemolytic anemia Hereditary Spherocytosis Red cell metabolic enzyme defects Defects in membrane skeleton proteins— hereditary spherocytosis Defects in enzymes involved in energy production—GP6D deficiency Defects in hb structure or synthesis-- Defects in spectrin or ankyrin People tend to be of European background Blebs are pinched off by macs in spleendecreased size of cell, lose biconcavity Symptoms: splenomegaly, ankle ulcers, pigmented gallstones, INCREASED OSMOTIC FRAGILITY, increased MCHC Tx: folate, splenectomy has a risk for OPSS overwhelming post-splenectomy sepsis Aerobic metab requires G6PD. This is required for detoxification of oxidative stress and getting rid of methemoglobin Heinz bodies methoglobin that denatures and ppcs out Type B=most prevelant, Type A=20% of healthy Af-Ams have this. Af. Mutant A- unstable and loses activity; Mediteranian always low base activity X-linked Clincal features: triggered by drugs, infections, maximal 7-10d of drug exposure Tx: avoid oxidant agents, folate repletion Oxidant drugs/chemicals which cause hemolysis Sulfa drugs, chloramphenicol Dapsone Quinine and chloroquine, primiaquine Vitamin K Fava beans Naptha compounds--mothballs •antibodies bind to red cellsRE system via Fc R’spherocyte formation 1. warm antibody mediated—drug induced, reacts at 37’, does not cause red cell agglutination. IgG 2. cold antibody mediated—react best <32’, do cause red cell agglutination. IgM Hallmark: positive coomb’s test Immune mediated hemolysis Two types? Hallmark? Coomb’s test Causes of autoimmune hemolytic anemia Clinical Features of autoimmune hemolytic anemia? Tx? Myeloid Looks for antibodies to red cells, comes as a set: 1. Directpt’s RBC’s with goat-anti-human IgG or C3 inkit 2. indirecttest for IgG or C3 inserum Busulfan Idiopathic Complication of SLE, lymphoma, or leukemia Infections can provoke it Drugs can induce it Associated with immune platelet destruction— Evan’s syndrome Thiotepa Fatigue Pallor Jaundice Splenomegaly Lab: increased reticulocyte, increased bilirubin, increased LDH, positive coombs, sphereocytes Tx: immunosuppression1. corticosteroids, 2. splenectomy, 3. cyclophosphamide Drug induced hemolytic anemias Cold agglutinin disease/autoimmune hemolytic anemia. Tx? Carmustine (BCNA Innocent bystander mechanism antibodies + drug land on RBCsRE system clears; drug must be present Hapten mechanism antibodies against durg + RBC suface True autoimmune mechansism antibody production continues even in absence of drug Dacarbazine— IgM!! Directed against I or i antigen Agglutinatecyanosis or ischemia in the cold extremities. Coombs is + for C3, negative for IgM Etiology: IgM, Mycoplasm pneumonia, Mononucleoisis, lymphoproliferative disease Tx: cold avoidance, mittens, folate repletion Microangiopathic Hemolytic anemia (MAHA) Neutorphils Lymphocytes Elevated neutrophil count Neutropenia Non-immune Hallmark: schistocytes-scharp Chemotaxis, phagocytosis, killing of phagocytosed bacteria Fine pink granules Adherance rolling mediated by selectins, firm adhesion via beta-2 integrins Recognition and phagocytosis, make phagosome Degranulation Oxidative metabolism and bacterial killing. First NADH oxidase converts superoxide into hydrogen peroxide. Within phagosome, myeloperoxidase combines hydrogen peroxide and chloride to form hydrochlorous acid Immune regulation Hematopoitic growth factors Physiologic: Neonate, Exercise, Lactation, Pregnancy Acute infection or inflammation Acute hemorrhage Non-hemolytic malignancies Myeloproliferative diseases Metabolic: uremia, acute thyrotixicosis, diabetic ketodosis Drugs: G-CSF, GM-CSF, corticosteroids, lithium Seizures, electric shock Post-splenectomy Rebound after neutropenia Drugs: antipsycotics, antiepileptics, propylthiouracil (anti-thyroid), gold salts, sulfa drugs, chemotherapy Infections Immune: SLE, Felty’s syndrome Familial/congenital Endocrine hyperthyroidism, hyperpituitarism Felty’s syndrome Rheumatoid arthritis Splenomegaly neutropenia Eosinophilia Neoplasia Allergic disorders Addison’s disease Collagen Vascular disease Parasites Basophilia Hypersensitivity reactions Chronic myeloproliferative diseases Thyroid disease Lymphocytosis Viral infections Bacterial infections CLL (chronic lymphocytic leukemia) lymphomas immunodeficiencies immunosuppressive drugs lymphomas granulomatous disease, including TB and sarcoidosis alcoholism malnutrition zinc deficiency lymphocytopenia monocytosis LAD Chronic granulomatous disease Chediak-Higashi syndrome Acquired defects in neutrophil function bacterial infections: TB, syphilis, bucellois, SBE, typhoid!! Protozoa infections Rickettsial infections—incl. rocky mountain spotted fever Myelodysplastic features Leukemias Other malignancies Inflammatory bowel disease Neutorphils lack beta2 integrins for surface adhesion, unable to leave circulation Peripheral WBC count is ELEVATED because they can’t leave Recurrent infections with lack of pus X linked defect in components of NADPH oxidase complex Recurrent pyrogenic infections with organisms that are catalase positivedegrades H2O2 Eg staph aureus (has Exotoxin F, TSS) Autosomal Recessive defects in granule fusion with plasma membrane Defects in leukocyte function, platelet function Deaths in early childhood CALM Corticosteroid use Alcoholism Leukemias Myelodysplasia Myeloproliferative syndrome