management of diabetic ketoacidosisin the emergency room
advertisement

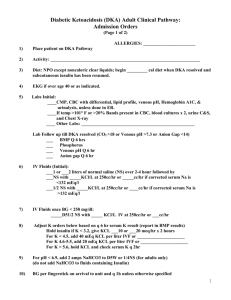
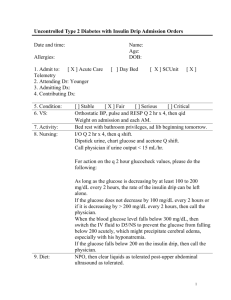
DKA GUIDELINES (revised, March 2004) The diagnosis should be made on the basis of: 1. History 2. Physical examination 3. Ketonemia and/or ketonuria 4. Serum glucose > 300 mg/dl by a bedside glucometer and confirmed by laboratory testing. 5. Acidosis: venous pH < 7.3, arterial pH < 7.35, venous H2CO3 < 18 mEq/L Note: The Patient can have severe hyperglycemia but not have ketoacidosis and vice versa, i.e., the patient can be in ketoacidosis even though the serum glucose may be < 250 (Euglycemic Diabetic Ketoacidosis) These guidelines are intended for the management of the following children : - more than 5% dehydrated - and/or vomiting - and/or drowsy - and/or clinically acidotic (usaully venous pH < 7.2) MANAGEMENT OF DIABETIC KETOACIDOSIS IN EMERGENCY ROOM 1. The patient should be started on an IV of 0.9% normal saline (NS) at the rate of 20cc/kg/hr. 2. Consider nasal oxygen. 3. Identify precipitation factor and rule out surgical condition. MANAGEMENT OF DIABETIC KETOACIDOSIS IN HOSPITAL. 1. I.V. Hydration: a. 0.9% NS, 20 ml/kg/hr for the first two hours. (adjust for the fluid already given in the Emergency Room, and/or clinic) DO NOT rebolus the patient with 20 ml/kg/hr of NS simply because the patient still seems dehydrated after the initial bolus; such a condition should be expected. Rebolusing should only be performed after consultation with attending. b. After 2 hours of 0.9% NS, the IV fluid should be changed to 0.45% NS. Calculate the total fluid requirement for 24 hours: Total fluid requirement (maintenance and deficit) in 24 hours = 3.5L/m2 regardless of degree of dehydration. From total fluid requirement, subtract the amount of fluid given in the first two hours; the remainder should be given in the next 22 hours. Example IV rate for next 22 hours (cc/hour) = 3500 x surface area (m2) – (20 ml/kg x 2 hour) 22 (hour) If the estimated maintenance and deficit fluid exceeds this calculation, the rest will be replaced after first 24 hours. add K+ after urine output is established, serum K < 5.5 mEq/L and no peaked T waves on the ECG serum K+ <3.5 mEq/L add 60 mEq/L + serum K 3.5-5.5 mEq/L add 40 mEq/L If anuria is suspected but serum K+ < 3 mEq/L, add K+ 30 mEq/L. Use half as KCL and half as potassium phosphate (1 mEq of K+ from KCL to 1 mEq of K+ from potassium phosphate). c. When the bedside blood glucose (BG) level reaches 300 mg/dl or less, change the IV fluid to D 5, 0.45% NS with K+. If the BG level tends to fall below 100 mg/dl, the IV fluid may need to be changed to D 10 or even 12.5% with 0.45% NS and with K+. Do not discontinue the insulin drip until the patient is out of DKA d. Do not replace the amount passed in the urine. Discuss with attending if urine output is greater than hourly intake. 2. Insulin Treatment: Insulin treatment should be started AFTER the first two hours of hydration are completed. Prior to starting insulin Rx, obtain VBG, Chemistry panel, and bedside BG. a. Start a separate IV line for the Insulin Drip and infuse insulin at the RATE of 0.1 unit/kg/hr (1 cc/kg/hr) (Preparation of solution for IV Insulin Infusion: Add 50 units of regular Human insulin to 500 cc of 0.45% NS) Run 50 ml of insulin solution through IV tubing to saturate insulin binding sites. In an individual who has received insulin and injection of insulin within the past 6 hours, consider using a lower dose of insulin 0.05 units/kg/hr for the first few hours. b. Regulate decline in BS: 50-100 mg/dl per hour AFTER insulin drip. Do not decrease the insulin drip below 0.05 units/kg/hour unless the patient is out of DKA. BG usually falls between 50-200 mg/dl from redehydration in the first1-2 hour without insulin therapy. c. If BG < 300 follow 1c Do not discontinue the insulin drip until the patient is out of DKA (venous pH >7.3, or HCO3 > 15) d. There is no need to subtract the amount of insulin solution from Total fluid requirement in 1b. e. Prepare a fresh, I.V. insulin drip solution drip solution every 6 hours. 3. Alkali Therapy No HCO3 is required, irrespective of the severity of the acidosis. Please discuss with attending if the patient is profoundly acidotic (pH< 7.0) and shocked with circulatory failure. MONITORING: Monitor the following parameters during treatment : 1. Bedside BG q 1-2 hour e.g. q 1 hour for 8 hours, then q 2 hour if clinically stable. 2. Chemistry panel and venous blood gases q 2-4 hour e.g. q 2 hour for 4-8 hours, then q 4-6 hour until the acidosis is resolved. Monitor serum calcium, and phosphate if severe acidosis Monitor serum Mg if previously abnormal or hypocalcemia. Any abnormalities in serum K+, corrected Na+ , Ca2+ , Mg2+ or phosphate should be discussed with attending immediately. Consider change concentration of NS and K+ to correct serum K+ and corrected serum sodium level Cerebral edema 1. Beware of alarming Neurological signs and symptoms and write orders to monitor hourly during treatment and for 24 hours after recovery the following: - Severe headache - Arousal, sensorium and behavioral change - Papillary changes - Bradycardia - Urinary incontinence - Seizures - Disturbed body temperature regulation The attending should be notified, at once, of the development of any of these problems. The following measures should be taken Give Mannitol 0.5 g/kg stat (= 2.5 ml/kg Mannitol 20% over 15 minutes). This needs to be given as soon as possible. Restrict IV fluids to 2/3 maintenance and replace deficit over 72 hours. The child will need to be moved to ICU (if not there already) if necessary arrange for the child to be intubated and hyperventilated to reduce blood pCO2 (controversial). Elevate head of bed. Inform neurosurgeons Exclude other diagnoses by CT scan - other intracerebral events may occur (thrombosis, haemorrhage or infarction) and present in the same way Intracerebral pressure monitoring may be required RECOVERY PHASE: When the venous blood gas is corrected to venous pH 7.3, or more, with a PCO2>35 and a HCO3, of 18 or more, the patient has recovered from it at that level until the time of the next meal; monitor the blood only if they are indicated. Follow the guideline for “What to do after recovery from DKA” for ongoing therapy. The patient is kept NPO until recovery from DKA has been achieved. Continue with IV fluids until the child is drinking well and able to tolerate food. Do not expect ketones to have disappeared completely before changing to subcutaneous insulin. Discontinue the insulin infusion 30 minutes after the first subcutaneous injection to allow time for the subcutaneous injection to start working. Mild Diabetic Ketoacidosis If a child has mild DKA (venous pH>7.2) and is taking oral fluid, insulin (0.2-0.25 units/kg/dose) can be admisnistered SC or IM every 4-6 hours. Subsequent doses are adjusted depending on the response to the previous injection and the blood glucose prior to the injection. Consider ICU admission for 1 altered mental status 2 age less than 2 years with pH < 7.25 3 blood glucose > 1000 mg/dl Admission guildline in acute metabolic complications of diabetes. (ADA, 1997) Admission is appropriate for the following: Diabetic ketoacidosis Blood glucose >250 mg/dl (>13.9 mmol/l) with 1) arterial pH <7.35, venous pH <7.30, or serum bicarbonate level <15 mEq/l and 2) ketonuria and/or ketonemia. Hypoglycemia with neuroglycopenia 1) Blood glucose <50 mg/dl (<2.8 mmol/l) and the treatment of hypoglycemia has not resulted in prompt recovery of sensorium; or 2) coma, seizures, or altered behavior (e.g., disorientation, ataxia, unstable motor coordination, dysphasia) due to documented or suspected hypoglycemia; or 3) the hypoglycemia has been treated but a responsible adult cannot be with the patient for the ensuing 12 h; or 4) the hypoglycemia was caused by a sulfonylurea drug. Corrected serum sodium = serum sodium + (serum glucose – 100) x 1.6 100 Since there is a greater risk for cerebral edema in hypernatremic dehydration. (corrected serum sodium > 150 mEq/L), the sodium should be gradually corrected. Revised March 4, 2004