Give an account of the basic and clinical pharmacology of drugs
advertisement

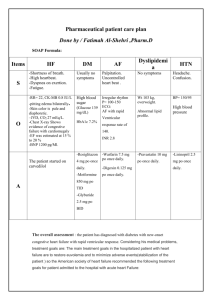
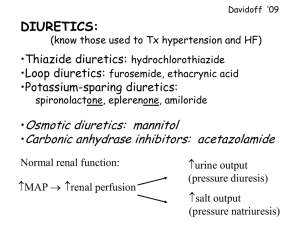
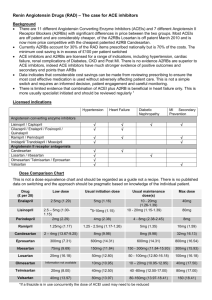
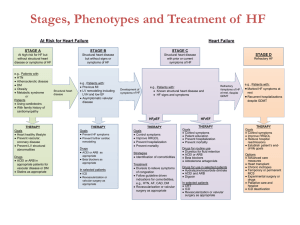
Give an account of the basic and clinical pharmacology of drugs used to manage HEART FAILURE. The underlying abnormality in heart failure is a cardiac output that is inadequate to meet the metabolic demands of the body during exercise, and ultimately also at rest. It may be caused by disease of the myocardium itself, most commonly ischaemic heart disease, or by circulatory factors such as volume overload or pressure overload. When cardiac output decreases, an increase in fluid volume occurs, causing sodium and water retention via the activation of the renin-angiotensin-aldosterone system. Irrespective of the cause, outlook for adults with heart failure is grim; 50% of those with the most severe grades are dead within 6 months. Non-drug measures, including the restricting of dietary salt are important, but ultimately drugs are needed to improve the symptoms of oedema, fatigue, and breathlessness and also to improve prognosis. The treatment of chronic heart failure aims to relieve symptoms, improve the exercise tolerance of the patient, reduce the incidence of acute exacerbations and reduce mortality. Drugs used in the treatment of heart failure include Angiotensin Converting Enzyme inhibitors (ACEi), Diuretics, Digoxin, ß-adrenoceptor antagonists, spironolactone and Angiotensin Receptor Blockers (ARBs). ACEi ACEi have a valuable role in all grades of heart failure, combined when appropriate with a diuretic and digoxin. The rennin-angiotensin-aldosterone system is inappropriately activated in patients with heart failure. ACEi counteract this. By blocking the formation of Angiotensin II, they reduce vascular resistance, improving tissue perfusion and reducing cardiac afterload. They also cause natriuresis by inhibiting the secretion of aldosterone and reducing the direct stimulatory effect of Ang II on reabsorption of sodium and bicarbonate in the early part of the proximal convoluted tubule. ACEi are best avoided in patients with known or suspected reno-vascular disease. In patients with sever bilateral renal artery stenosis, ACEi reduce or abolish glomerular filtration and are likely to cause severe and progressive renal failure. Renal function and electrolytes should be checked before starting ACEi and monitored during treatment. 1 Concomitant treatment with NSAIDs increases the risk of renal damage; via tubular necrosis. ACEi should be used with caution in patients receiving diuretics; first doses may cause profound hypotension. Side effects of ACEi include hypotension and renal impairment. They may also cause angioedema, rash, persistent dry cough, pancreatitis and upper respiratory symptoms. Several ACEi are now in use and they include enalapril, lisinopril, ramipril, perindopril and trandolapril. ARBs although not licensed for the treatment of heart failure, may be used in patients for whom ACEi are contraindicated due to the persistent cough. Diuretics Loop diuretics are used in pulmonary oedema due to left ventricular failure; iv administration produces relief of breathlessness and reduces preload sooner than would be expected from the time of onset of diuresis. Loop diuretics are also used in patients with longstanding heart failure. These drugs act primarily on the thick segment of the ascending Loop of Henle inhibiting the transport of NaCl out of the tubule into the interstitial tissue by inhibiting the Na+/K+/2Cl- carrier in the luminal membrane. Loop diuretics are readily absorbed from the GI tract and may also be given by injection. They are strongly bound to plasma protein and so do not pass into the glomerular filtrate to any marked degree. Given orally they act within one hour and if given by iv the act within 30 minutes. Unwanted effects of loop diuretics include hypokalaemia, hypotension and metabolic acidosis. Digoxin Digoxin is given to patients in atrial fibrillation and also to those in sinus rhythm who remain symptomatic despite treatment with an ACEi and a diuretic. The main mechanisms of action of cardiac glycosides, like digoxin, are increased vagal activity and inhibition of the Na+/K + pump. Digoxin slows the AV conduction by increasing vagal activity via an action on the CNS. Digoxin also causes a large increase in twitch tension in isolated preparations of cardiac muscle. The effects of digoxin are increased if plasma [K +] decreases because of reduced competition at the K + binding site of the Na+/K + ATPase. This fact is important clinically as 2 diuretics which decrease potassium are often used in conjunction with digoxin; this can lead to an increased risk of dysrhythmia. ß-adrenoceptor antagonists Heart failure is accompanied by potentially harmful activation of the sympathetic nervous system as well as the rennin-angiotensin-aldosterone system, providing a rationale for the use of ß-adrenoceptor antagonists. Most doctors are wary of this approach because of the negative inotropic action of these drugs. However when they are started in low doses which are increased slowly, metoprolol, carvedilol and bisoprolol have been shown convincingly to improve survival. Spironolactone The aldosterone antagonist, spironolactone, may be considered for patients with sever heart failure who are already receiving an ACEi, a diuretic and possibly digoxin. Low doses of spironolactone have been shown to reduce symptoms and mortality in these patients. Spironolactone is well absorbed from the GI tract and its plasma t½ is only around 10 minutes, however its active metabolite canrenone has a t½ of 16 hours. GI upsets occur fairly frequently and spironolactone used on its own can cause hyperkalaemia and possibly metabolic acidosis. Finally, in the treatment of acute, severe heart failure, dobutamine can be given by iv infusion. This drug stimulates ß1-adrenoceptors in the heart and increases contractility with little effect on the rate. It is used in refractory patients or those awaiting cardiac transplantation. Heart failure exists when cardiac output is insufficient to adequately perfuse the tissues. The low cardiac output in heart failure results in increased sympathetic nervous activity; which stimulates the rate and force of the heartbeat and maintains the BP by increasing vascular resistance. In the failing heart, the resulting increase in the resistance against which the heart has to pump further decreases cardiac output. With combinations of ACEi, diuretics, digoxin, spironolactone and careful use of ß-adrenoceptor antagonists, one hopes to relieve symptoms and reduce mortality. 3