Renin Angiotensin Drugs - NHS Stockport Clinical Commissioning
advertisement

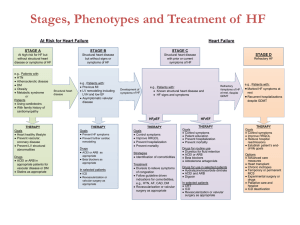
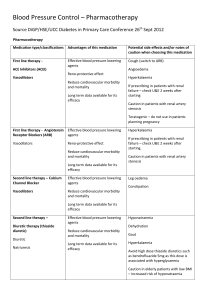
Renin Angiotensin Drugs (RAD) – The case for ACE inhibitors Background There are 11 different Angiotensin Converting Enzyme Inhibitors (ACEIs) and 7 different Angiotensin II Receptor Blockers (A2RBs) with significant differences in price between the two groups. Most ACEIs are off patent and are considerably cheaper, of the A2RBs Losartan is off patent March 2010 and is now more price competitive with the cheapest patented A2RB Candesartan. Currently A2RBs account for 30% of the RAD items prescribed nationally but is 70% of the costs. The minimum cost saving is in excess of £100 per patient switched ACE inhibitors and A2RBs are licensed for a range of indications, including hypertension, cardiac failure, renal complications of Diabetes, CKD and Post MI. There is no evidence A2RBs are superior to ACE inhibitors, indeed ACE inhibitors have much stronger evidence of positive outcomes and secondary end points than ARBs Data indicates that considerable cost savings can be made from reviewing prescribing to ensure the most cost effective medication is used without adversely affecting patient care. This is not a simple switch and requires an informed decision, patient engagement and careful monitoring. There is limited evidence that combination of ACEI plus A2RB is beneficial in heart failure only. This is more usually specialist initiated and should be reviewed regularly 1 Licensed indications Hypertension Heart Failure Diabetic Nephropathy MI Secondary Prevention Angiotensin converting enzyme inhibitors Lisinopril / Captopril Cilazapril / Enalapril / Fosinopril / Quinalapril Ramipril / Perindopril Imidapril/ Trandolapril / Moexipril Angiotensin II receptor antagonists Candesartan Losartan / Irbesartan Olmesartan/ Telmisartan / Eprosartan Valsartan Dose Comparison Chart This is not a dose equivalence chart and should be regarded as a guide not a recipe. There is no published data on switching and the approach should be pragmatic based on knowledge of the individual patient. Drug (£ per 28) Low dose Usual initiation dose Enalapril 2.5mg (1.29) 5mg (1.16) Lisinopril 2.5 – 5mg (1.001.15) 2mg (2.29) Perindopril *5-10mg (1.15) Usual maintenance dose(s) 10 - 20mg (1.26-1.39) 10 - 20mg (1.15-1.39) Max dose 40mg 80mg 4mg (2.38) 4 - 8mg (2.38-2.45) 8mg Ramipril 1.25mg (1.17) 1.25 - 2.5mg (1.17-1.26) 5mg (1.35) 10mg (1.59) Candesartan 2 – 4mg (13.67-9.25) 8mg (9.98) 8mg (9.98) 32mg 16.13) Eprosartan 300mg (7.31) 600mg (14.31) 600mg (14.31) 800mg (16.54) Irbesartan 75mg (9.69) 150mg (11.84) 150 - 300mg (11.84-15.93) 300mg (15.93) Losartan 25mg (16.18) 50mg (12.80) 50 - 100mg (12.80-16.18) 100mg (16.18) Olmesartan Information not available 10mg (10.95) 10 – 20mg (10.95-12.95) 40mg (17.50) Telmisartan 20mg (8.00) 40mg (12.50) 40 -80mg (12.50-17.00) 80mg (17.00) Valsartan 40mg (13.97) 80mg (13.97) 80-160mg (13.97-18.41) 160 (18.41) *If a thiazide is in use concurrently the dose of ACEI used may need to be reduced Action Plan Suggested process Identify all patients on A2RBs and ACEI Identify all patients on ARB2 Then identify those 1. who have never had an ACEI Actions required and Rationale Agreement By When whom Review each case to ensure use is appropriate in light of current guidance on lack of benefit in any condition except heart failure Invite any patients who are non concordant to attend for review with a view to engagement and assessment of need, if re initiating ensure the most appropriate drug e.g. ACEI is selected Review each patient with a view to exclude patients with drug interaction or where switching would pose an unjustifiable risk. For the remainder implement a managed switch to formulary ACEI and ensure appropriate monitoring/ dose titration. 2. who have Review drug choice. For patients with hypertension for cough recorded as ADR 3. who are not on a formulary ARB2 Identify all patients on ACEI Audit effectiveness of the programme whom an ACE was 1st choice but suffered intractable cough, is an A2RB the right drug. Consider if a thiazide or Ca channel blocker could be used. Age may be relevant if the patient is now over 55. Review drug choice in light of current formulary advice. If appropriate switch to a more cost effective A2RB Invite any patients who are non concordant to attend for review with a view to engagement and assessment of need; if re initiating ensure the most appropriate ACEI is selected. Review drug choice for any patient not on a formulary ACEI. Ensure ramipril is prescribed as caps and perindopril as the erbutamine salt Data collection and review A template is available from the NPC Exclusion criteria for switching Recorded / validated adverse reaction to ACEI which resolved on stopping and did not occur on ARB2 Patients whose clinical condition is unstable and change could result in serious adverse effects/ hospital admission. So what about cough? In trials a low percentage discontinue ACEI as a result of intractable cough (2-10%). Not all coughs require that the ACEI be stopped and the cough does not always resolve on an A2RB as cough is a common symptom in patients with heart failure or who smoke. The absolute incidence for the ONTARGET trial indicated a difference of just 3.1% between ACEI and A2RB. Or put it another way if 100 people take an A2RB instead of an ACEI only 3 will avoid having to stop the medication because of a cough and another one will stop whether they had the A2RB or an ACEI.