Pharmaceutical patients care plan
advertisement
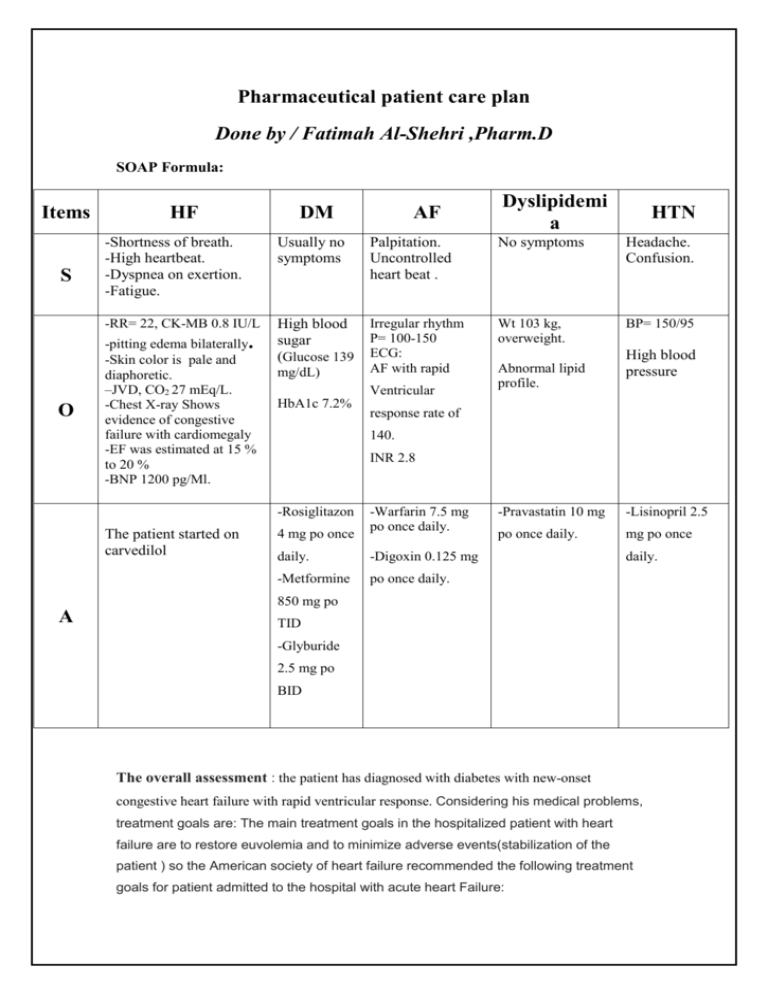
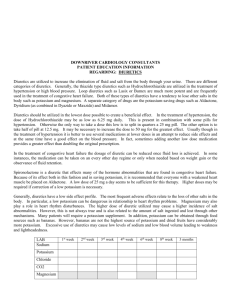
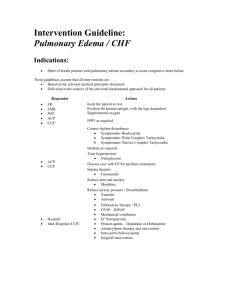
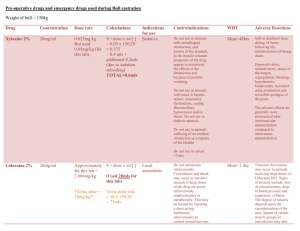
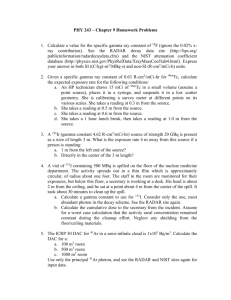
Pharmaceutical patient care plan Done by / Fatimah Al-Shehri ,Pharm.D SOAP Formula: Items S O HF DM AF Dyslipidemi a HTN -Shortness of breath. -High heartbeat. -Dyspnea on exertion. -Fatigue. Usually no symptoms Palpitation. Uncontrolled heart beat . No symptoms Headache. Confusion. -RR= 22, CK-MB 0.8 IU/L High blood sugar (Glucose 139 Irregular rhythm P= 100-150 ECG: AF with rapid Wt 103 kg, overweight. BP= 150/95 -pitting edema bilaterally. -Skin color is pale and diaphoretic. –JVD, CO2 27 mEq/L. -Chest X-ray Shows evidence of congestive failure with cardiomegaly -EF was estimated at 15 % to 20 % -BNP 1200 pg/Ml. mg/dL) Ventricular HbA1c 7.2% High blood pressure response rate of 140. INR 2.8 -Rosiglitazon The patient started on carvedilol Abnormal lipid profile. 4 mg po once -Warfarin 7.5 mg po once daily. daily. -Digoxin 0.125 mg -Metformine po once daily. -Pravastatin 10 mg -Lisinopril 2.5 po once daily. mg po once daily. 850 mg po A TID -Glyburide 2.5 mg po BID The overall assessment : the patient has diagnosed with diabetes with new-onset congestive heart failure with rapid ventricular response. Considering his medical problems, treatment goals are: The main treatment goals in the hospitalized patient with heart failure are to restore euvolemia and to minimize adverse events(stabilization of the patient ) so the American society of heart failure recommended the following treatment goals for patient admitted to the hospital with acute heart Failure: 1-improvement of symptoms especially (congestion,shortness of breath ,dysnea,and low output symptoms ). 2-Optimize volume status(decrease edema ). 3-Restore normal oxygenation. 4-Identify and address the precipitating factors . 5-Optimize chronic oral therapy . 6-Minimize the side effects . the medications that are indicated in the long-term management of this patient’s heart failure are usually : Common in-hospital treatments include intravenous diuretics, vasodilators, and inotropic agents. But In the long term management of heart Failure strategies differ according to whether or not the patient has significant systolic dysfunction, but in general for any patient with heart Failure after stabilization according to the guidelines we use : -ACEI or ARBs. -BB.(not in the acute HF). -And if the patient is overloaded(edema) we add : ACEI+BB+Loop diuretics. The drugs, doses, schedules, and duration for the management of this patient? For management of his heart Failure - we use ACEI (e.g:Captopril 6.25mg/day as a starring dose, and the target dose is :50mg TID. -BB and the best in this case is: -Carvedilol :3.125mg/day as a staring dose then increase toward the target dose which is :25mg BID. Because the patient has hypertension and heart failure so we prefer carvedilol as BB coz it has Alpha activity (it means that will help to reduce the hypertension due to it's activity on alpha receptors inducing dilatation ) . From diuretics : we use loop diuretics , Furosemide:20-40mg/day as a stating dose and a maximum dose is 600mg/day . ACEI+BB should be used long life ,but diuretics only if the patient is edematous ,and once the patient is improved no need to use it . The most common precipitants for HF hospitalization are: - noncompliance with medications or dietary restrictions. - uncontrolled hypertension, ischemia, arrhythmias. -exacerbation of chronic obstructive pulmonary disease with or without pneumonia. -Other contributors include noncardiac conditions such as renal dysfunction, diabetes mellitus, anemia, and the side effects of medications (nonsteroidal anti-inflammatory drugs, calcium-channel blockers, and thiazolidinediones). So the patient has DM we should monitor his blood glucose to insure that the DM is controlled .The patient also has AF and he's on warfarin ,and digoxin ,we should monitor the digoxin level routinely to make sure that the level is in the theraputic window . The patient also on furosemide and the most common side effect is electrolyte imbalance so we should monitor the hypokalemia which is a major cause of digoxin toxicity . Rosiglitasone (that is used for DM ) can cause fluid retention and peripheral edema. As a result, it may precipitate congestive heart failure (which worsens with fluid overload in those at risk)so it's better to use another anti diabetic or to decrease the dose of rosiglitasone. Thiazolidinediones, including pioglitazone and rosiglitazone, cause or exacerbate congestive heart failure in some patients. (After initiation of these drugs, as well as after dose increases, observe patients carefully for signs and symptoms of heart failure (including excessive, rapid weight gain; dyspnea; and/or edema); if these signs or symptoms develop, the heart failure should be managed according to the current standards of care; furthermore, discontinuation or dose reduction of these drugs must be considered. These drugs are not recommended for patients with symptomatic heart failure; initiation of these drugs in patients with established NYHA class III or IV heart failure is contraindicated). Metformin: Patients with CHF requiring pharmacologic management, in particular those with unstable or acute CHF who are at risk for hypoperfusion and hypoxemia, are at an increased risk for lactic acidosis; the risk for lactic acidosis increases with the degree of renal dysfunction and the patient’s age,so we should take this in our consideration . The plan: -Stabilization of the patient,and restoration of heart functions and elimination of exx fluid. -Monitoring of INR, digoxin level and electrolytes to prevent any adverse effects that could happened from diuretic therapy and other medications. -Monitoring of potassium level. -Monitor the patient's blood pressure because it wasn’t controlled. -Monitoring of liver function tests because the patient is on pravastatin which may cause hepatotoxicity and rhabdopmyolysis. -Changing the ant diabetic rosiglitazone or decrease its dose until the patient is stabilized and monitoring the lactic acidosis because the patient is on metformin .