Diuretics
advertisement
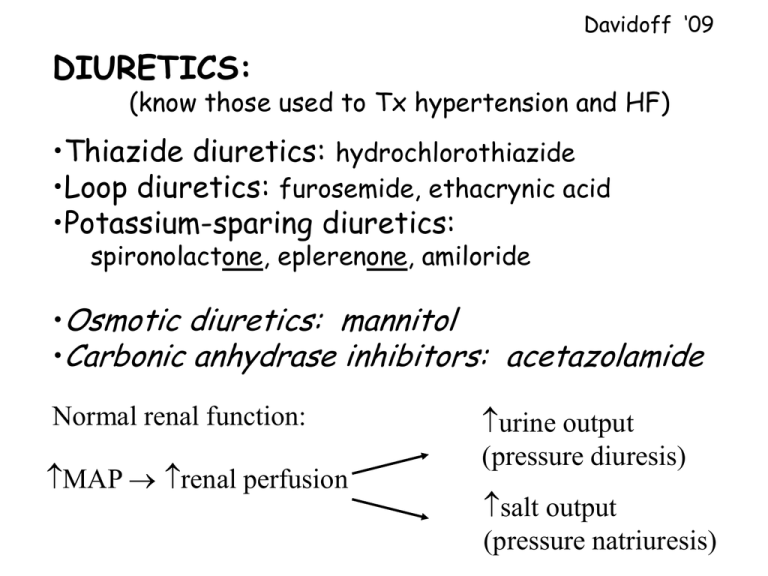
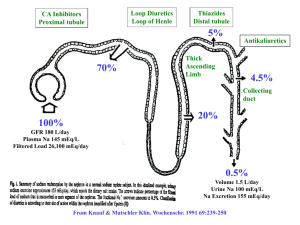
Davidoff ‘09 DIURETICS: (know those used to Tx hypertension and HF) •Thiazide diuretics: hydrochlorothiazide •Loop diuretics: furosemide, ethacrynic acid •Potassium-sparing diuretics: spironolactone, eplerenone, amiloride •Osmotic diuretics: mannitol •Carbonic anhydrase inhibitors: acetazolamide Normal renal function: MAP renal perfusion urine output (pressure diuresis) salt output (pressure natriuresis) Rationale for using diuretics For heart failure: Blood volume preload (cardiac work) congestion (edema) For hypertension: Blood volume and peripheral resistance preload (ventricular filling) CO BP • Diuretics promote natriuresis (Na+ excretion) • Water tends to follow Na+ (diuresis) • Relative potencies of diuretics: Loops >> Thiazides >>>>>> K+ sparing + Na Ca2+ reabsorption Thiaz filtration Na+ secretion Na+ +ALD K+ H+ Loops +ADH Katzung Fig 15-1 K+ sparing Thiazides: hydrochlorothiazide •Most commonly used class of diuretics •Differ in their pharmacokinetics •Indicated for mild hypertension short-term effects blood volume long-term effects TPR (lose their diuretic effects) •For moderate or severe hypertension, used in combination with other antihypertensive drugs •Flat dose-response curve (i.e., increasing dose does not make them more effective) loss of diuresis is fast Brenner Fig 10-2 Thiazides: (con’t) •Na+ reabsorption by inhibiting Na/Cl co-transport in the distal convoluted tubule •Modest effect because only 5-10% of Na+ is reabsorbed there •Must be filtered or secreted to work, therefore ineffective in patients with renal insufficiency/failure •Require renal prostaglandins to work, therefore NSAIDs can interfere with diuresis Side effects: •Hypokalemic metabolic alkalosis •Blood glucose, lipids, and uric acid Bonus: Blood Ca2+ (via Ca2+ reabsorption) Urine Ca2+ With whom should care be taken? useful for osteoporosis useful for kidney stones Na+ How do thiazides (and loops) promote K+ loss? collecting duct tubular Na+ Na+ Na+ K+ H loss K+ H Loss Na+/K+ exchange urine urine Loop diuretics: furosemide, ethacrynic acid • “High ceiling diuretics” - work in a dose-dependent manner • Ethacrynic acid is an alternative if patient has sulfonamide allergy • Extremely effective, rapid onset • Indicated for severe edema (e.g., pulmonary edema, CHF) not typically used for hypertension • Inhibit Na/K/2Cl transport in ascending loop of Henle normally responsible for ~35% Na+ reabsorption • Are filtered and secreted • Directly increase renal blood flow, therefore effective with renal insufficiency Diuresis 'high ceiling diuretics' 'flat D-R curve' Dose of diuretic Brenner Fig 13-3 Like Thiazides: Loops require renal prostaglandins to work, therefore NSAIDs can interfere with diuresis Side effects include: • Hypokalemic metabolic alkalosis and hyperuricemia • Hypovolemia • Ototoxicity Loops greater incidence of adverse side effects than thiazides + Na Ca2+ reabsorption Thiaz filtration Na+ secretion Na+ +ALD K+ H+ Loops +ADH Katzung Fig 15-1 K+ sparing Potassium sparing ‘diuretics’ Spironolactone, Eplerenone, Amiloride • Weak diuretics used in combination with other diuretics • Antagonize aldosterone effects • Aldosterone is a steroid binds to mineralocorticoid receptors in tubular epithelial cells stimulates the synthesis of Na/K/H pumps promotes Na+ reabsorption, K+/H+ secretion • Prevents hypokalemia from thiazide and loop diuretics • Must be cautious of hyperkalemia Spironolactone • Competitively binds to aldosterone receptors - nonselective (mineralocorticoid, androgenic and progesterone receptors) • Inhibits aldosterone-induced synthesis of pumps • Slow onset (WHY?), long duration (active metabolites) • Weak naturiuretic effects, but lowers BP in some patients with mild/moderate hypertension • Also indicated for hyperaldosteronemia • Shown to improve morbidity and mortality in patients with end-staged heart failure (Pitt et al., NEJM, 1999) Side effects include: Men: gynecomastia and erectile dysfunction because of anti-androgenic actions Women: menstrual irregularities, hirsutism Eplerenone • More specific for aldosterone receptors than spironolactone therefore avoids side effects (but really expensive) • Currently approved hypertension and post-MI LV dysfunction • CYP450 3A4 inhibitors (e.g., erythromycin, verapamil, and grapefruit juice) can elevate blood levels of eplerenone Aldosterone is also associated with endothelial dysfunction and fibrotic effects in hypertension, HF and atherosclerosis (mechanism underlying ACE-I cardioprotection???) Cardioprotective effects appear similar to spironolactone http://www.jaapa.com/issues/j20040201/articles/0204wcardiomeds.html Amiloride •Directly inhibits pumps in distal tubules and collecting ducts therefore independent of aldosterone (blocks Na+ selective channels in apical membrane) •Onset of action much faster than spironolactone does not involve gene expression •Relatively few side effects (caution about hyperkalemia) JNC VII Compelling Indications for Drug Classes Initial Therapy Options Clinical-Trial Basis Heart Failure Diuretic, BB, ACEI, ARB, Aldo Ant MERIT-HF, COPERNICUS, CIBIS, SOLVD, AIRE, TRACE, Val-HeFT, RALES Post-MI BB, ACEI, Aldo Ant ACC/AHA Post-MI Guideline, BHAT, SAVE, Capricorn, EPHESUS High CAD Risk Diuretic, BB, ACEI, CCB Compelling Indication Diabetes Mellitus Chronic Kidney Disease Recurrent Stroke Prevention Diuretic, BB, ACEI, ARB, CCB ACEI, ARB Diuretic, ACEI ALLHAT, HOPE, ANBP2, LIFE, CONVINCE NKF-ADA Guideline, UKPDS, ALLHAT NKF Guideline, Captopril Trial, RENAAL, IDNT, REIN, AASK PROGRESS ACEI=Angiotensin converting enzyme inhibitor, Aldo Ant=Aldosterone antagonist, ARB=Angiotensin receptor blocker, BB=b-blocker, CAD=Coronary artery disease, CCB=Calcium channel blocker, MI=Myocardial Infarction Chobanian AV et al. JAMA. 2003;289:2560-2572