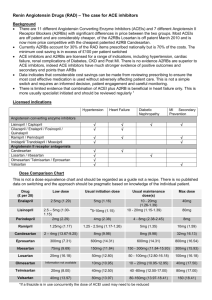
Congestive heart failure
advertisement
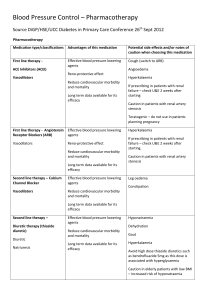
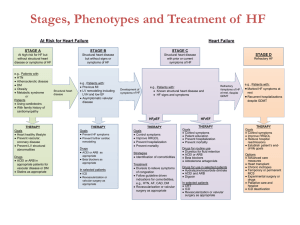
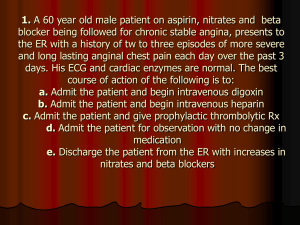
Vilasinee Hirunpanich B.Pharm, M.Sc In Pharm (Pharmacology) Congestive heart failure Definition Systolic dysfunction ผลจากการที่กล้ามเนื้อหัวใจไม่ สามารถสูบฉีดเลือดไปเลี้ยงเนื้อเยือ่ ต่างๆ ได้เพียงพอกับความ ต้องการของร่ างกาย Diastolic dysfunction กล้ามเนื้อหัวใจไม่สามารถ คลายตัวรองรับเลือดเข้าสู่หวั ใจได้ดีพอ อาการแสดง Dypnea Fatigue Fluid retention Shortness of breath สาเหตุของการเกิด heart failure Decrease cardiac output Compensatory mechanisms 1. Extrinsic compensatory 2. Intrinsic compensatory Extrinsic compensatory Increase the sympathetic system HR, contraction Stimulate renin-angiotensin system aldosterone Sodium and Water retention Intrinsic compensatory Frank-Starling mechanism Myocardial hypertrophy remodeling Left Ventricular cannot pump blood ลด Cardiac output Intrinsic compensatory Extrinsic compensatory เพิ่มcontractility เพิ่มsympathetic discharge vasoconstriction เพิม่ afterload Ventricular hypertrophy HR ลดrenal perfusion เพิ่มการหลัง่ renin AT II aldosterone Fluid retention เพิ่ม preload Failure compensatory mechanism อาการที่เกิดขึน้ หากเกิดการล้ มเหลวของ compensatory mechanism Management of heart failure Prevention of initial causative Pharmacological treatment Hemodynamic model (1950-1980) increase contractility Treatment – Conventional drugs • Diuretic • Digitalis • vasodilators Neurohormone model (1980-2000) Progressive remodeling with impaired myocardial performance Treatment – Conventional drugs – Decreasing the process of cardiac remodeling (ACEI, -blocker, nitrate) – Neurohormone blockers • ACEI (RAAS) • Spironolactone (aldosterone) • -blocker (renin) • Digoxin (renin) Treatment of CHF Goal: to relief symptom 1. Control salt and water retention (diuretic) 2. Increase myocardial contractility (inotropic drugs) 3. Reduce work load of heart by Preload: Diuretic, Nitrate, ACEI Afterload: Direct vasodilator Decrease activation of neurohormone: ACEI, -blocker, spironolactone Heart failure vasodilator Decreased cardiac output Increased venous volume and pressure Decreased tissue perfusion Neuroendocrine system activation Congestion and edema Dysnea and orthopnea Positive inotropic Sympathetic activation RAS vasoconstriction Na retention Increased afterload Positive inotropic drugs Cardiac glycoside Digitalis, digoxin, quabain Non-cardiac glycoside – Phosphodiesterase inhibitors (PDEI) – Catecholamine (Dopamine, Dobutamine) Cardiac glycoside Digoxin is the prototype. Digitalis lanata, Digitalis purpurea Digoxin, digitoxin, quabain Lactone ring and steroid nucleus are essential for activity sugar molecule influence pharmacokinetic Pharmacological effects 1. Positive inotropic effect Glycoside Inh. Of Na+/K+ ATPase Decrease Na+/Ca2+ exchange Increase cardiac [Ca2+] Increase contraction Positive inotropic effect (cont) Binding with Na+/K+ ATPase thus inhibit Na+ pump – 20-40 % inhibition – >50 % inhibition therapeutic toxic Increase the force of contraction of both normal and failure heart. Improvement hemodynamic in failure heart. 2.Sensitized baroreceptor reflex Parasympathetic activation AV-node inhibition, increase refractory period Sympathetic inhibition – Inhibit sympathetic discharge – Inhibit renin release 3. Decrease electrical activity Decrease action potential depolarization Decrease conduction velocity 4. Other effects Muscle – Slightly increase Ca2+ in muscle GI – N/V, stimulate CTZ (vomiting center) CNS – Disorientation, hallucination, convulsion Pharmacokinetics Absorption Variable oral bioavailability depend on dosage form – 70% tablet – 85% elixir – 95% capsule 10% of pts. metabolism by Eubacterium lentum Distribution Vd 7-8 L/kg Little affinity for distribution into fat (dosing should base on ideal body weight) Myocardial/serum digoxin concentration ratio are approximately 30:1. Hypokalemia increase the binding of digoxin to heart. Metabolism Enterohepatic recycling Gut bacterial enzyme conjugation Excretion Renal route T1/2 1.6 day Pts with renal disease increase T1/2 3.5-4.5 d. Therapeutic concentration Drug has narrow therapeutic index. Therapeutic range 0.5-2 ng/ml (after 4-5 T1,/2) Dose adjustment when drug reach to steady State. (equilibrium between heart and serum) ADR GI N/V, vomiting, diarrhea, abdominal pain, constipation Neurologic Headache, fatigue, insomnia, vertigo Visual Color vision (green or yellow), colored halos around the subject Miscellenoues Allergic, thrombocytopenia, necrosis ADR (cont) Heart SA and AV node suppression AV block Atrial arrhythmia Ventricular arrhythmia Risk of treatment Serum digoxin level > 2 ng/ml – Cardiac arrhythmia – GI symptom – Neurogenic compliant Lower digoxin level is toxic if hypokalemia, hypomagnesemia and hypercalcemia. Comcomittent use of quinidine, verapamil, flecainide and amiodarone which increase digoxin level. Clinical Use To improve clinical status of the patient Combination with -blocker, diuretic, ACEI 1.catecholamine 2. PDEI Catecholamine Dopamine 1, 1 DA receptor Increase NE… tachycardia Dobutamine synthetic analoge of dopamine Stimulate 1> 2 receptor and > receptor (not DA receptor) positive inotropic Use in refractory HF, sever acute MI, cardiotonic shock PDEI (phosphodiesterase enzyme inhibitor) Bipyridine derivatives – Amrinone, milrinone, vesnarinone Pharmacological actions Positive inotropic effect Peripheral vasodilation Coronary vasodilation Mechanism of PDE inhibitors Drug inhibit PDE enz. Increase cAMP heart Vascular smooth muscle เพิ่ม Ca2+ influx เพิ่ม Ca2+ efflux ลด Ca2+ efflux ลด Ca2+ influx HR vasodilation ADR Cardiac arrhythmia Hypotension N/V Amrinone………. Thrombocytopenia, liver enzyme Milirinone…….. Bone marrow suppression, liver toxicity Vasodilators Reduce preload/afterload Venodilator…Isosorbide, nitroglycerine Vasodilator….hydralazine, minoxidil, Ca2+ channel blocker Both Venodilator and Vasodilator……ACEI, prazosin ACEI ACEI in CHF – Report that reduce remodeling – Reduce aldosterone from the compensatory mechanism – Vasodilate (Preload/after load) Improve symptoms and clinical status and decrease the risk of death and hospitalization in mild, moderate, severe heart failure. Decrease risk of HF in pts with LV-dysfunction ACEI in CHF Contraindicated in Angioedma Anuric renal failure Pregnancy Use with caution in pts with Serum K+> 5.5 mmole/L Diuretic Goal: decrease edema and pulmonary congestion เพิ่มการขับน้ าออกจากร่ างกาย, ลด blood volume Thiazide diuretic, loop diuretic, K+ sparing diuretic Loop diuretic ใช้ในกรณี ที่มี CO ลดลงรุ นแรงและใช้ thiazide ไม่ได้ผลแล้ว (GFR <30 ml/min) Diuretic+ACEI/-blocker > monotherapy (will stimulate RAAS) ข้อควรระวังในการใช้ diuretic ในการรักษา CHF Electrolytes depletion Serious cardiac arrhythmia Add K+ sparing diuretic Neurohormonal activation increase activation of RAAS Add ACEI Hypotension Excessive use Worsening heart failure beta-blockers Effect in CHF – Block SNS effects – Block renin Improve symptoms and clinical status Combination with diuretic, ACEI, digoxin, vasodilators Bisoprolol, metoprolol, Carvedilol Risk of treatment Hypotension Fluid retention & worsening CHF Bradycardia & heart block Contraindication in pts with CHF exacerbation Aldosterone antagonist Spironolactone Research study indicate that spironolactone reduce mortality and morbidity in CHF. Monitor K+ level.