Mechanical Ventilation LAB and in class work
advertisement
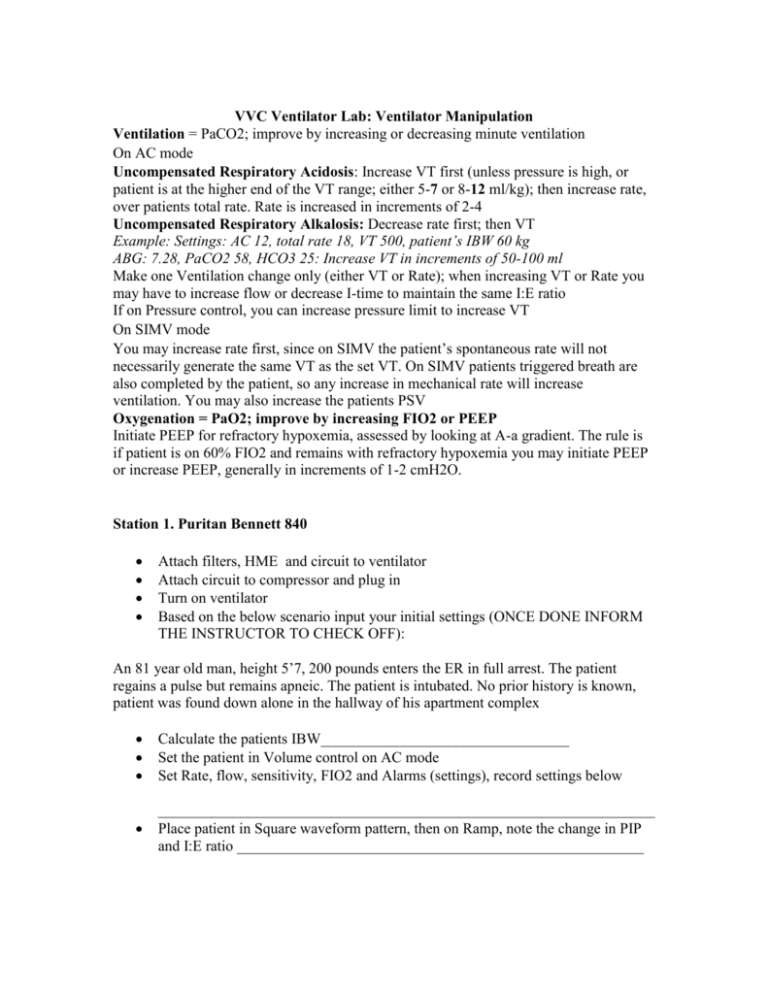
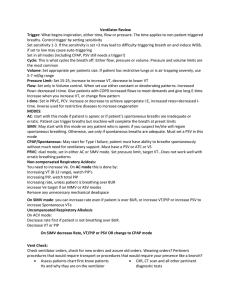
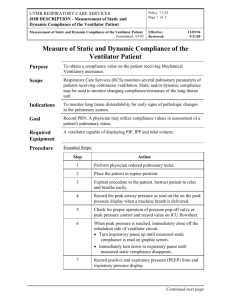
VVC Ventilator Lab: Ventilator Manipulation Ventilation = PaCO2; improve by increasing or decreasing minute ventilation On AC mode Uncompensated Respiratory Acidosis: Increase VT first (unless pressure is high, or patient is at the higher end of the VT range; either 5-7 or 8-12 ml/kg); then increase rate, over patients total rate. Rate is increased in increments of 2-4 Uncompensated Respiratory Alkalosis: Decrease rate first; then VT Example: Settings: AC 12, total rate 18, VT 500, patient’s IBW 60 kg ABG: 7.28, PaCO2 58, HCO3 25: Increase VT in increments of 50-100 ml Make one Ventilation change only (either VT or Rate); when increasing VT or Rate you may have to increase flow or decrease I-time to maintain the same I:E ratio If on Pressure control, you can increase pressure limit to increase VT On SIMV mode You may increase rate first, since on SIMV the patient’s spontaneous rate will not necessarily generate the same VT as the set VT. On SIMV patients triggered breath are also completed by the patient, so any increase in mechanical rate will increase ventilation. You may also increase the patients PSV Oxygenation = PaO2; improve by increasing FIO2 or PEEP Initiate PEEP for refractory hypoxemia, assessed by looking at A-a gradient. The rule is if patient is on 60% FIO2 and remains with refractory hypoxemia you may initiate PEEP or increase PEEP, generally in increments of 1-2 cmH2O. Station 1. Puritan Bennett 840 Attach filters, HME and circuit to ventilator Attach circuit to compressor and plug in Turn on ventilator Based on the below scenario input your initial settings (ONCE DONE INFORM THE INSTRUCTOR TO CHECK OFF): An 81 year old man, height 5’7, 200 pounds enters the ER in full arrest. The patient regains a pulse but remains apneic. The patient is intubated. No prior history is known, patient was found down alone in the hallway of his apartment complex Calculate the patients IBW_________________________________ Set the patient in Volume control on AC mode Set Rate, flow, sensitivity, FIO2 and Alarms (settings), record settings below __________________________________________________________________ Place patient in Square waveform pattern, then on Ramp, note the change in PIP and I:E ratio ______________________________________________________ One hour later an ABG is obtained with the following results: pH 7.28 PaCO2 67 PaO2 167 HCO3 29 BE 2.8 Correct the above ABG by making the appropriate changes to the ventilator (ONCE DONE INFORM THE INSTRUCTOR) Changes made: _________________________________________________________ After your changes Calculate the patients RAW __________________________ Obtain a Static and Dynamic Compliance Cs__________________________________________________________________ Cd_________________________________________________________________ Perform a expiratory pressure hold ________________________ Change the patient to SIMV mode, set PSV (above calculated RAW), decrease the rate Monitor the following and record the results: PIP __________________ MAP _________________ Ve ___________________ I:E ratio _______________ VTe__________________ Go to plot setup and select Flow/time and Pressure/time Trigger a breath and note appearance of trigger on graphic Change graphic to Pressure/volume and draw appearance in space below Change patient to Spontaneous mode, initiate PEEP. (note in this mode you will have to stimulate breaths) Note changes to MAP when PEEP is added. Also note baseline pressure change in the Pressure/time graphic WHEN FINISHED, DIASSEMBLE VENTILATOR CIRCUIT AND FILTERS FOR THE NEXT GROUP Station 2: Gaileo ventilator Attach filters, HME and circuit to ventilator Attach circuit to compressor and plug in Turn on ventilator Based on the below scenario input your initial settings (ONCE DONE INFORM THE INSTRUCTOR TO CHECK OFF): A 27 year old man, height 5’10, 187 pounds enters the ER in status asthmaticus. The patient is in severe respiratory distress and is intubated. Calculate the patients IBW_________________________________ Set the patient in Pressure Control on AC mode Set Rate, I-time, sensitivity, FIO2 and Alarms (settings), record settings set below __________________________________________________________________ Set I time to achieve a I:E of 1:4, set I-time ______________________________ One hour later an ABG is obtained with the following results: pH 7.68 PaCO2 27 PaO2 56 HCO3 22 BE -2.8 Correct the above ABG by making the appropriate changes to the ventilator (ONCE DONE INFORM THE INSTRUCTOR) Changes made: _________________________________________________________ After your changes Calculate the patients RAW __________________________ Obtain a Static and Dynamic Compliance Cs__________________________________________________________________ Cd_________________________________________________________________ Perform a expiratory pressure hold ________________________ Change the patient to SIMV mode, set PSV (above calculated RAW), decrease the rate Monitor the following and record the results: PIP __________________ MAP _________________ Ve ___________________ I:E ratio _______________ VTe__________________ Note the pattern on the Flow/time and Pressure/time graphic Trigger a breath and note appearance of trigger on graphic Change graphic to Flow/volume and draw appearance WHEN FINISHED, DIASSEMBLE VENTILATOR CIRCUIT AND FILTERS FOR THE NEXT GROUP Station 3: Espirit Ventilator Attach filters, HME and circuit to ventilator Attach circuit to compressor and plug in Turn on ventilator Based on the below scenario input your initial settings (ONCE DONE INFORM THE INSTRUCTOR TO CHECK OFF): A 42 year old, 185 pound man, 5’8 tall, with advanced Myasthnia Gravis is admitted for progressing weakness. A MIP is performed and indicates a value of -18. The patient is therefore intubated with a size 6.0 ETT after difficulty by the RT to intubate. Calculate the patients IBW_________________________________ Set the patient in Pressure Control on SIMV mode Set Rate, I-time, sensitivity, FIO2, PSV and Alarms (settings), record settings set below __________________________________________________________________ Set I time to achieve a I:E of 1:3, set I-time ______________________________ Which parameter would you want to assess with a patient with a size 6.0 ETT? __________________________________ One hour later an ABG is obtained with the following results: pH 7.28 PaCO2 58 PaO2 120 HCO3 26 BE 1.2 Correct the above ABG by making the appropriate changes to the ventilator (ONCE DONE INFORM THE INSTRUCTOR) Changes made: _________________________________________________________ After your changes Calculate the patients RAW __________________________ Obtain a Static and Dynamic Compliance Cs__________________________________________________________________ Cd_________________________________________________________________ Perform a expiratory pressure hold ________________________ Change the patient to AC mode Monitor the following and record the results: PIP __________________ MAP _________________ Ve ___________________ I:E ratio _______________ VTe__________________ Note the pattern on the Flow/time and Pressure/time graphic Trigger a breath and note appearance of trigger on graphic Change graphic to pressure/volume and draw appearance WHEN FINISHED, DIASSEMBLE VENTILATOR CIRCUIT AND FILTERS FOR THE NEXT GROUP Station 4: In class work 1. Explain the procedure for a minimal leak technique 2. Explain what a MAP is and the factors that can increase it 3. Draw a flow/time graph with Auto-PEEP, label inspiration, expiration and the point of air trapping 4. How can you decrease auto-peep in VC and PC? 5. Draw a pressure/volume loop for a patient on Volume control with over distention 6. What are the indications of PEEP? What are the side effects 7. What will occur if sensitivity level is set to high? Too low? 8. When is PEEP initiated? 9. What is the normal range for VC, MIP, MEP, RAW, Cs and Cd For the following scenario, place the patient on initial ventilator settings 10. 89 year old, 5’8, with known respiratory acidosis, currently apenic, no other lung disease. 11. Patient with pulmonary fibrosis, and a PaO2 40 on room air. 12. When would you place a patient on non-invasive ventilation as opposed to invasive? 13. During mechanical ventilation what parameter would you adjust first in order to correct a respiratory acidosis? 14. Describe what happens to Inspiratory time when flow is increase 15. What is the benefit of a constant flow pattern over a decelerating ramp? 16. What are some ways we could prevent or ease “bucking” or asynchrony with mechanical ventilation? Calculate the following formulas based on the scenario below A 180 pound, 5’9, 56 year old man is intubated with a size 8.0 ETT. He is placed on AC mode with a rate of 12, VT 550, 40% FIO2 and PEEP 5 ABG: pH 7.30, PaCO2 52, PaO2 80, HCO3 20, BE -2 VBG: pH 7.26, PvCO2 60, PvO2 32, HCO3 22, BE -1.6 Na+ 150 K+ 5.5 Cl- 90 HCO3 26 Hb 10 Cardiac Output 4L Inspiratory time 1.25 seconds, Expiratory time 3.25 seconds PIP 36 Plateau pressure 32 17. CaO2 18. CvO2 19. VO2 20. A-a gradient 21. Flow 22. VA 23. TCT 24. I:E ratio 25. Suction catheter size 26. Anion Gap 27. Desired PaCO2 of 40; calculate New rate: New VT: 28. Desired PaO2 of 90; calculate New FIO2: 29. RAW 30. CD 31. CS 32. a/A ratio 33. MAP A patient on SIMV mode with a set rate of 8 and total rate of 12, VT 500, PSV 10, and FIO2 50%. Minute volume is 8 L 34. Calculate patients Spontaneous Ve 35. Calculate patients Spontaneous VT