ARDS_CLINICAL ALGORITHM
advertisement
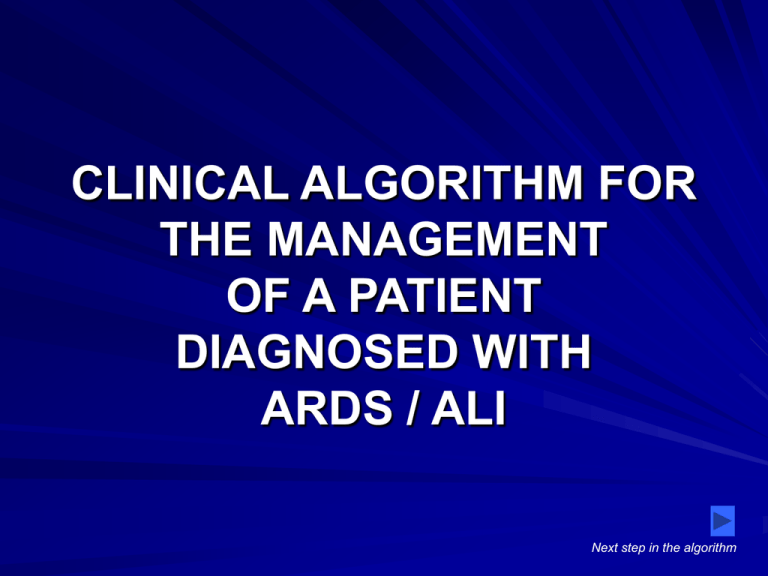
CLINICAL ALGORITHM FOR THE MANAGEMENT OF A PATIENT DIAGNOSED WITH ARDS / ALI Next step in the algorithm On evaluation Patient presents with PaO2: FiO2 <27 KPa/ 200mmHg Bilateral changes visible on CxR Of acute onset PAWP <18 Non - cardiogenic PaO2: FiO2 >27 KPa/ 200mmHg < 40kPa / 300mmHg Next step in the algorithm CONTRA INDICATIONS present ? cerebral perfusion pressure of less than 60 mm Hg, Intracranial pressure of more than 30mmHg massive hemoptysis, broncho-pleural fistula, tracheal surgery or sternotomy in the last 15days, MAP of less than 65mmHg with or without vasopressors, deep venous thrombosis pacemaker inserted for fewer than 2 days, unstable fracture; (Guerin et al 2004) Open chest or abdominal wounds, advanced pregnancy, and severe facial trauma or recent ophthalmic surgery NO YES EXPERT OPINION Leone 2002; Rowe 2004 Develop a PATIENT SPECIFIC MOBILITY PLAN in consultation with multidisciplinary team members Monitor patient closely: and Only suction when clinically indicated – Coarse breath sounds; noisy breathing; increased or decreased pulse; increased or decreased respiration; increased or decreased blood pressure; prolonged expiratory breath sounds; clinically apparent increased work of breathing – Use VHI two hyperinflations using the CPAP function of the ventilator to an airway pressure of 45cmH2O for 20 s, with an interval of 1 min in between and after suction procedure RECOMMENDATION 2 Back to algorithm Initiate discussion with multidisciplinary team Consider the following PRACTICAL CONSIDERATIONS Have access to an appropriate pressure-relieving surface Patient is adequately sedated and receiving muscle relaxants Have a pulse oximeter to monitor heart rate and oxygen saturation Sufficient number of staff available to turn patient (initiate and after 6 hours) EXPERT OPINION (Ball et al 2001; McCormick et al 2001; Rowe 2004) Not in place In place Develop a PATIENT SPECIFIC MOBILITY PLAN in consultation with multidisciplinary team members Monitor patient closely: and Only suction when clinically indicated – Coarse breath sounds; noisy breathing; increased or decreased pulse; increased or decreased respiration; increased or decreased blood pressure; prolonged expiratory breath sounds; clinically apparent increased work of breathing – Use VHI two hyperinflations using the CPAP function of the ventilator to an airway pressure of 45cmH2O for 20 s, with an interval of 1 min in between and after suction procedure RECOMMENDATION 2 Back to algorithm TURN PT PRONE: PREPARATIONS Temporarily halt the patients’ enteral feed and aspirate nasogastric tube. Position a sliding sheet in situ Secure the endotracheal/tracheostomy tube. Make sure appropriate intubation equipment is immediately available Suction patient Disconnect infusion lines, naso-gastric feeds and ECG pads. Lines / tubes deemed essential by its continued presence must be adequately secured and flexible enough to accommodate all aspects of the turn. Direct the lines towards the patients’ head, Ensure that the eyelids remain closed at all times and appropriate lubrication instilled RECOMMENDATION 1 Previous step in the algorithm Next step in the algorithm TURN PT PRONE: PROCEDURE Position pillows across pt chest, pelvis and knees Ensure patients’ arms are positioned close to their sides, with the palms facing inwards One staff member manages the head and tracheal tube and two members on either side of patient Pull bottom sheet straight and taut and lay a second sheet across the patient, ensuring that all corners are matching, effectively cocooning the patient and pillows inside. Move the patient towards one side of the bed. Roll slowly onto flank and then onto abdomen in the direction of the ventilator. Position head facing towards the ventilator. Reconnect the equipment. EXPERT OPINION Ball et al 2001; McCormick et al 2001; Rowe 2004; Alsaghir et al 2008 Previous step in the algorithm Next step in the algorithm Check immediately for ADVERSE REACTIONS cardiac arrest, unplanned extubation, endotracheal tube obstruction, hemoptysis, transcutaneous oxygen saturation [SpO2] <85% for more than 5 minutes, heart rate_<30/min for more than 1 minute, arterial systolic blood pressure <60 mm Hg for more than 5 minutes, No adverse reactions Pt demonstrates adverse reactions Immediately return patient to supine and address appropriately management Previous step in the algorithm POSITION PATIENT Upper pillow must support the patients’ upper chest, allowing their shoulders to fall forwards slightly The middle pillow should be positioned under the patients’ pelvis, thus maintaining them in an abdomen-free position Maintain the patient within the swimmers position, ensuring that their face looks towards the prominent arm, the opposite one being positioned carefully down by their side Shoulder position of the prominent arm must be maintained at 80° abduction, whilst the elbow is flexed to 90° In addition, a small-rolled pillowcase should be placed in the palm of the prominent hand to extend the wrist and allow flexion of the fingers. Once established in the prone position, place the bed in a reverse Trendelenburg position, i.e. tilted foot down 30–45° EXPERT OPINION Ball et al 2001; McCormick et al 2001; Rowe et al 2004 Previous step in the algorithm Next step in the algorithm After 6 hours PaO2:FiO2 increased by at least 20mmhHg RECOMMENDATION 1 NO YES • Return to supine position and manage as non responder management Previous step in the algorithm Continue in prone position for at least 8 hours to a maximum of 20 hours RECOMMENDATION 1 Continue for at least 7 days (Rowe 2004; Alsaghir et al 2008) META ANALYSIS Back to algorithm