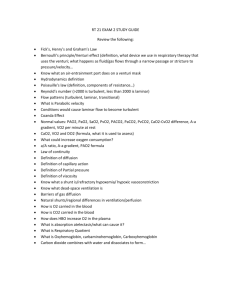
RT 230 PPP-Unit A and Unit B

RT 230
Unit A-
Indication, Setup and Monitoring of CMV
I NDICATIONS FOR CMV
Apnea
Acute ventilatory failure: A PCO
2 of more than
50mmHg with a pH of less than 7.25
Impending acute ventilatory failure
Based on lab data and clinical findings indicating that pt is progressing towards ventilatory failure
Quick tip: acute hypercapnic failure ph drops 0.8 for every
10mm hg rise in co2 chronic hupercapnic ph drops 0.03 for every 10 mmhg rise in co2
Clinical problems often resulting in impending ventilatory failure
Pulmonary abnormalities
RDS=Respiratory Distress Syndrome
Pneumonia
Pulmonary emboli
Mechanical ability of lung to move air=muscle fatigue
Ventilatory muscle fatigue
Chest injury
Thoracic abnormalities=scoliosis, kyphoscoliosis
Neurologic disease=GB, MG
Pleural disease=pleurasy
Clinical evaluation
Vital signs: Pulse and BP increase
Ventilatory parameters
V
T decreases
RR increases
Accessory muscle use increases
Paradoxical breathing (abdomen out, rib cage in)
Retractions may be noted
Development of impending acute vent failure may demonstrate
Progressive muscle weakness in pt with Neurologic disease
Increasing fatigue
ABGs demonstrating a trend toward failure
9am10am 11am 12pm 1pm pH 7.58 7.53 7.46 7.38 7.35
PCO
2
HCO
3
PO
2
22
21
60
28
22
55
35
23
50
42
24
43
48
24
40
Non-responsive hypoxemia
PaO
2
less than 50% on an FIO greater than 50%
2
PEEP is indicated
REFRACTORY HYPOXEMIA
P HYSIOLOGIC E FFECTS OF P OSITIVE P RESSURE
V ENTILATION
Increased mean intrathoracic pressure
Decreased venous return
Thoracic pump is eliminated***
Pressure gradient of flow to right side of heart is decreased
Right ventricular filling is impaired
Give fluid
Decreased cardiac output
Caused by decreased venous return
Give drugs and fluid
Monitor I and O. Normal urine output 1000-1500 cc/24 hours
THORACIC PUMP
The "thoracic pump" is the thoracic cavity, the diaphragm, the lungs, and the heart.
The diaphragm moves down, pressure in the cavity decreases and venous blood rushes through the vena cava via the right heart into the lungs. Pulmonary blood vessels expand dramatically, filling with blood, air and blood meeting across the very thin alveolar surface.
The deeper the inhalation, the more negative the pressure, the more blood flows, and the fuller the lungs become.
THORACIC PUMP
As the diaphragm moves up the pressure in the thoracic cavity reverses. Pulmonary blood vessels shrink ejecting an equal volume of blood out of the pulmonary veins into the left heart. The left heart raises the pressure and checks and regulates the flow. The more complete the
exhalation
, the more positive the pressure becomes and the more blood is ejected from the lungs.
Decrease exhalation, more pressure in cavity decrease CO
E FFECTS OF PPV CONT .
Increased intracranial pressure
Blood pools in periphery and cranium because of decreased venous return
Increased volume of blood in cranium increases intracranial pressure
Decreased urinary output
PPV could cause 30-50% decrease renal output
Decreased CO results in decreased renal blood flow
Alters filtration pressures and diminishes urine formation
Decreased venous return and decreased atrial pressure are interpreted as a decrease in overall blood volume
ADH is increased and urine formation is decreased
ADH=VASOPRESSIN
Roughly 60% of the mass of the body is water, and despite wide variation in the amount of water taken in each day, body water content remains incredibly stable. Such precise control of body water and solute concentrations is a function of several hormones acting on both the kidneys and vascular system, but there is no doubt that antidiuretic hormone is a key player in this process.
Antidiuretic hormone, also known commonly as arginine vasopressin
The single most important effect of antidiuretic hormone is to conserve body water by reducing the loss of water in urine. A diuretic is an agent that increases the rate of urine formation.
high concentrations of antidiuretic hormone cause widespread constriction of arterioles, which leads to increased arterial pressure.
Retention of fluids will cause EDEMA
E FFECTS OF PPV CONT .
Decreased work of breathing
Force to ventilate is provided by the ventilator
Increased deadspace ventilation
Positive pressure distends conducting airways & inhibits venous return
The portion of V
T that is deadspace increases
Greater percentage of ventilation goes to apices
Increased intrapulmonary shunt
Ventilation to gravity dependent areas is decreased
Perfusion to gravity dependent areas increase
Shunt fraction increases from 2-5% to 10%
A pulmonary shunt is a physiological condition which results when the alveoli of the lung are perfused with blood as normal, but ventilation (the supply of air) fails to supply the perfused region. In other words, the ventilation/perfusion ratio (the ratio of air reaching the alveoli to blood perfusing them) is zero. A pulmonary shunt often occurs when the alveoli fill with fluid, causing parts of the lung to be unventilated although they are still perfused
.
Intrapulmonary shunting is the main cause of hypoxemia (inadequate blood oxygen) in pulmonary edema and conditions such as pneumonia in which the lungs become consolidated.
The shunt fraction is the percentage of blood put out by the heart that is not completely oxygenated. A small degree of shunt is normal and may be described as 'physiological shunt'. In a normal healthy person, the physiological shunt is rarely over 4%; in pathological conditions such as pulmonary contusion , the shunt fraction is significantly greater and even breathing 100% oxygen does not fully oxygenate the blood.
[1]
E FFECTS OF PPV CONT .
Respiratory rate, V
T
, Inspiratory time, and flow rate can be controlled
May cause stress ulcers and bleeding in GI tract
C OMPLICATIONS OF M ECHANICAL
V ENTILATION
Complications related to pressure
Ventilator-associated lung injury (VALI)
High pressures are associated with barotrauma
Pneumothorax, pneumomediastinum, pneumopericardium, subcutaneous emphysema
Pneumothorax has decreased chest movement, hyperresonance to percussion, on affected side
If tension pneumothorax: medical emergency
Relieved by needle insertion, then chest tube
Use 100% oxygen to speed reabsorption.
Placing patient on CMV
Establish airway
Select V
T
8-12ml/kg of ideal body weight
Select mode - a/c sensitivity at minimal to not self cycle
Set pressure limit 10cmH
2
O above delivery pressure
Set sigh volume 1-1/2 to 2 times V
T
Sigh pressure 10cmH
2
O above sigh delivery pressure
Rate as ordered
PEEP as ordered: exp. resist, insp. hold, etc.
Set spirometer 100 cc less than patient volume
check for function (turn on)
Modes
Control
All of WOB is taken over by ventilator
Sedation is required
Control mode is useful
During ARDS, especially if high PEEP is required or inverse
I:E ratio
Assist
Patient is able to control ventilatory rate
Should not be used for continuous mechanical ventilation if pt is apneic
Assist/control
Pt able to control vent rate as long as spontaneous rate > backup rate
Machine performs majority of WOB
Sedation is often required to prevent hyperventilation
Is useful during early phase of vent support where rest is required
Useful for long term for pt not ready to wean
SIMV
In between positive press breaths pt can breathe spontaneously
Useful for long term for pt not ready to wean
Used as weaning technique for short-term vent dependent pt
PS
Vent functions as constant pressure generator
Positive pressure is set
Pt initiates breath, a predetermined pressure is rapidly established
Pt ventilates spont, establishes own rate, V
T
I:E
, peak flow and
Can be used independently/CPAP/SIMV
Indicated to reduce work imposed by ETT, 5 to 20cm H
2
O
Can be used for weaning
A set IPS (12ml/kg VT) achieved by adjusting IPS level then slowly reducing as clinical status improves
To overcome resistance of ETT, IPS should meet Raw
To determine amount of PS needed: [(PIP – Plateau pressure) / Ventilatory inspiratory flow] x spontaneous peak inspiratory flow
IBW
Estimated ideal body weight in (kg)
Males: IBW = 50 kg + 2.3 kg for each inch over 5 feet.
Females: IBW = 45.5 kg + 2.3 kg for each inch over 5 fee.
1 Kilogram = 2.20462262 Pounds
M ONITORING CMV
Observation
Look at patient!
Make a good visual assessment
Start with patient, trace circuit back to ventilator
Check and drain tubing
Check connections
Check patient
Suctioning, position, etc.
BP
Spontaneous RR
Heart rate and all vital signs
Check machine settings
V
T
(set, exhaled, corrected)
f (assisted, set, spontaneous)
Pressure limit: 10 above delivery pressure
PEEP if applicable: Check BP!
Peak Insp. Pressure (PIP): Keep as low as possible
I:E ratio for proper flow
FiO
2
: Keep as low as possible to prevent Oxygen Toxicity yet keep them adequately oxygenated
Check all apnea alarms and settings.
Check set V
T
to exhaled V
T for any lost volumes
If difference is greater than 100 cc, check for leak.
Compliance
Measures distensibility of lung – how much does the lung resist expansion.
Relationship between Volume and
Pressure
High compliance equals lower PIP thus easier ventilation and less side effects of CMV
Disease states resulting in low compliance include the Adult Respiratory Distress Syndrome
(ARDS), pulmonary edema, pneumonectomy, pleural effusion, pulmonary fibrosis, and pneumonia among others.
Emphysema is a typical cause of increased lung compliance.
Y
OU MUST KNOW
Dynamic
= VT (corrected or exhaled)
PIP – PEEP
Always subtract out PEEP
Consistently use exhaled or corrected V
T
Used to assess volume/pressure relationships during breathing – any changes in RR will effect it
C
DYN decreases as RR increases which may cause V/Q mismatch which may cause hypoxemia
May reflect change due to change in flow due to turbulence instead of compliance
Normal = 30 – 40 cmH
2
O
V
ERY IMPORTANT
Static
= VT (corrected or exhaled)
Plateau – PEEP
Always subtract out PEEP
Always consistently use either V
T exhaled or V
T corrected
Will not change due to change in flow, more accurate
Measured pressure to keep airways open with no gas flow.
Normal values very with pt, but usually above 80 cmh2o will show lung overdistention
Importance
to follow trends in patient compliance
Decreased C = stiffer lung = less compliant = higher ventilating pressures = you need a ventilator with high internal resistance to deliver volumes using square wave.
High compliance = possible Emphysema
S TATIC VS D YNAMIC C OMPLIANCE
Decrease in C
DYN with no change in C worsening airway resistance
ST
indicates
Causes
Bronchospasm
Secretions
Kinked/Occluded ETT
Inappropriate flow and/or sensitivity settings
If both C
DYN problem
and C
ST worsen, not likely to be an airway
Causes
Pulmonary Edema
ARDS
Tension Pneumothorax
Atelectasis
Fibrosis
Pneumonia
Obesity
Patient Position
RAW = PIP – P plat
Flow (L/sec.)
Airway Resistance
Impedance to ventilation by movement of gas through the airways thus the smaller the airway the more resistance which will increase
WOB (causing respiratory muscle and patient fatigue)
Example: ETT, Ventilator Circuit,
Bronchospasm
Airway Resistance & Compliance
Decreased Compliance + Increased Airway
Resistance = High PIP, Decreased Volumes and significant increase in WOB
Very difficult to wean a patient until problems are resolved
P ATIENT STABILITY
Vital signs
Pulse – normal, weak, thready, bounding, rate, etc.
BP – hypo/hypertensive – directly related to CO
Respirations – tachypnea, bradypnea, hyperpnea, hypopnea, rate, etc.
Color – dusky, pale, gray, pink, cyanotic
Auscultation - bilateral, etc.
Are they bilateral, amount of air moving, rales, rhonchi or wheezing
Are they Vesicular (normal) or Adventitious (abnormal)
Describe what you hear: fine, course, high-pitched, lowpitched, etc.
And the location where you heard it: bilateral bases, posterior bases, right upper anterior lobe, laryngeal, upper airway, etc.
H EMODYNAMIC MONITORING
BTFDC
Also known as
Balloon Tipped Flow Directed Catheter
Swan-Ganz Catheter
Pulmonary Artery Catheter
Done by inserting a BTFDC into R atrium, thru R ventricle, and into pulmonary artery
SvO
2 is drawn from the distal port of a BTFDC
Used to monitor tissue oxygenation and the amount of O2 consumed by the body
C ATHETERS AND I NSERTION S ITES
PA P RESSURE W AVEFORMS
CVP
Monitors fluid levels, blood going to the right side of heart
Normal = 2 – 6 mmHg (4 – 12 cmH
2
O)
Increased CVP = right sided heart failure (cor pulmonale), hypervolemia (too much fluid)
Decreased CVP = hypovolemia (too little fluid), hemorrhage, vasodilation (as occurs with septic shock)
PAP
Pulmonary Artery Pressure = B/P lungs
Monitors blood going to lungs via Swan-Ganz catheter
(BTFDC)
Normal 25/8 (mmHg)
Increased PAP= COPD, Pulmonary Hypertension, or
Pulmonary Embolism
PCWP
Pulmonary Capillary Wedge Pressure monitors blood moving to the L heart
Balloon is inflated to cause a wedge
Normal PCWP = 8 mmHg
Range is 4 – 12 mmHg
Increased PCWP = L heart failure, CHF
Measure backflow resistance
Cardiac Output
Expressed as QT or CO (QT= Greek alphabet, 1050 BC scientist used qt had cardiac output expression)
Normal = 5 LPM
Range 4 – 8 LPM
Decreased CO = CHF, L heart failure, High PEEP effects
I & O
Needs to be monitored closely to prevent fluid imbalance due to increased ADH production and decreased renal perfusion
Fluid imbalance can develop into pulmonary edema and hypertension
C ARDIAC O UTPUT (CO)
The amount of blood pumped out of the left ventricle in 1 minute is the CO
A product of stroke volume and heart rate
Stroke volume: amount of blood ejected from the left ventricle with each contraction
Normal stroke volume: from 60 to 130 ml
Normal CO: from 4 to 8 L/min at rest
Fick CO: Vo2/Cao2-Cvo2
C(a-v)O2 could decrease if CO is increased due to less oxygen needs to be extracted from each unit of blood that passes
Fick Method
The Fick method requires that you be able to measure the A-V oxygen content difference and requires that you be able to measure the oxygen consumption. An arterial blood gas from a peripheral artery provides the blood for the
CaO2 measurement or calculation while blood from the distal PA port of a Swan-Ganz catheter provides the blood for the CvO2 measurement or calculation
Dilution methods mathematically calculate
(using calculus) the cardiac output based on how fast the flowing blood can dilute a marker substance introduced into the circulation normally via a pulmonary artery catheter.
(injecting a dye in prox port of Swanz. Not really used anymore due to infections
M EASURES OF C ARDIAC O UTPUT AND
P UMP F UNCTION
• C
ARDIAC INDEX
(CI)
•
Determined by dividing the
CO by body surface area
•
Normal CI is 2.5 to 4.0
L/min/m
2
•
CI measurement allows a standardized interpretation of the cardiac function
•
True cardiac output compared to each pers
ON
M EASURES OF C ARDIAC O UTPUT AND
P UMP F UNCTION ( CONT ’ D )
Cardiac work
A measurement of the energy spent ejecting blood from the ventricles against aortic and pulmonary artery pressures
It correlates well with the amount of oxygen needed by the heart
Normally cardiac work is much higher for the left ventricle
M EASURES OF C ARDIAC O UTPUT AND
P UMP F UNCTION ( CONT ’ D )
Ventricular stroke work
A measure of myocardial work per contraction
It is the product of stroke volume times the pressure across the vascular bed
Ventricular volume
Estimated by measuring end-diastolic pressure
Measures of Cardiac Output and
Pump Function (cont’d)
Ejection fraction
The fraction of end-diastolic volume ejected with each systole; normally 65% to 70%; drops with cardiac failure
D ETERMINANTS OF P UMP F UNCTION
Preload
Created by end-diastolic volume
The greater the stretch on the myocardium prior to contraction the greater the subsequent contraction will be
When preload is too low, SV and CO will drop
This occurs with hypovolemia
Too much stretch on the heart can also reduce SV
Determinants of Pump Function
Afterload
Two components: peripheral vascular resistance and tension in the ventricular wall
Created by end systolic volume
Increases with ventricular wall distention and peripheral vasoconstriction
As afterload increases, so does the oxygen demand of the heart
Decreasing afterload with vasodilators may help improve SV but can cause BP to drop if the blood volume is low
Ventilation Patient Parameters
Spontaneous V
T
Is it adequate for patient?
Spontaneous volumes should be between 5 – 8 ml/Kg of
Ideal Body Weight (IBW)
Spontaneous VC
10 – 15 ml/Kg IBW
NIF/MIP/MIF/NIP
-20 to -25 cmH
2
O within 20 seconds
ABG S
PaO
2 represents oxygenation – adjust with
PEEP or FiO
2
PaCO
2 or RR represents ventilation – adjust with V
T pH represents Acid/Base status
pH acid: High CO
2
(Metabolic cause)
(respiratory cause) or low HCO
3
pH alkaline: Low CO
2
(Metabolic cause)
(respiratory cause) or high HCO
3
Draw ABGs
To stabilize
With any change in ventilator settings change only one vent setting at a time
With any change in patient condition
V ENTILATOR ALARMS
Appropriate for each patient
Usually 10 higher/lower than set parameter
For pressure and RR settings
V
T alarms 100 ml higher/lower than set V
Adjust all alarms for patient safety.
T
XRAY WHEN INDICATED FOR
Tube placement: 2 – 4 cm above carina
Possible pneumothorax
To check for disease process reversal, or lack of, for treatment purposes and weaning
F REQUENCY OF VENTILATOR CHECKS
Must be done as often as required by the patients condition unstable patients continuous to hourly
In general patients and ventilators need evaluation Q1-Q4h
With every vent check, patient assessment should take place
Use VT exhaled for calculations.
Corrected VT = exhaled vt-tubing lost volume
Tubing volume lost factor 1-8 cc x pressure
Exhaled vt 650= pip-peep x (3) = 60
650-60=590 corrected vt
W AVEFORM A NALYSIS
Three wave forms typically presented together
Pressure
Flow
Volume
Plotted versus time
Horizontal axis is time
Vertical axis is variable
Other common wave forms:
Pressure vs Volume
Flow vs Volume
Pressure vs Time Assessment
Patient Effort: Negative pressure deflection at beginning of inspiration indicates patient initiated breath
Peak & Plateau Pressures
Adequacy of inspiratory flow: If pressure rises slowly, or if curve is concave, flow is inadequate to meet patient’s demand.
Flow vs Time Assessment
Inspiratory flow patterns
Air Trapping – a.k.a. AutoPEEP – expiratory flow fails to reach baseline prior to delivery of next breath
Airway Resistance
Lower slope (smaller angle) indicative of high resistance to flow
Steeper slope (greater angle) indicative of lower resistance to flow
Also increased resistance manifests itself as decreased peak expiratory flowrate (depth of expiratory portion of flow pattern) with more gradual return to baseline as expiratory flow meets with resistance
Bronchodilator = increased peak expiratory flow rate with quicker return to baseline
Volume vs Time Assessment
V
T
= peak value reached during inspiration
Air Trapping = fails to reach baseline before commencement of next breath
Identifying breath type
Larger volumes = mechanical breaths
Smaller volumes = spontaneous breaths
Pressure vs Volume Loop
Volume on vertical axis
Pressure on horizontal axis
Positive pressure on right of vertical axis
Indicates mechanical breath
Application of positive pressure to the lung
Tracing is in a “counter-clockwise” rotation
Subambient pressure to the left of the vertical axis
Indicates a spontaneous breath
Spontaneous inspiration is to the left of the vertical axis
– subatmospheric pressure at start of inspiration
(Intrapulmonary pressure = -3 cmH
2
O)
Spontaneous expiration is to the left of the vertical axis –
+3 cmH
2
O intrapulmonary pressure on expiration
Tracing is in a “clockwise” rotation
Useful in helping diagnosing
Alveolar Overdistension = looks like bird’s beak, or the
“Partridge Family” symbol
Increased R
AW
= looks “pregnant” or “fat”
Decreased compliance = looks “lazy” or like it’s lying down
Flow vs Volume Loop
Helpful in assessing changes in RAW, such as after the administration of a bronchodilator
Flow on vertical axis
Volume on horizontal axis
Inspiration is top part of loop, expiration on bottom
When R
AW improved, expiratory flows are greater and the slope of the expiratory flow is greater
To determine patient effort, use the following curves
Pressure vs Time
Pressure vs Volume Loop
Volume vs Time
All show subambient drops in pressure/volume when patient initiates the breath
To determine Auto-PEEP, use
Volume vs Time
Flow vs Time
Pressure vs Volume Loop
For all curves, ask “does the exhalation reach baseline before the next breath starts
To determine the adequacy of inspiratory flow
Pressure vs Time = concave or slow rise to pressure means inadequate flow on inspiration
Volume vs Time = Too slow flow = increased I – Time = decreased E-Time = AutoPEEP
Volume vs Pressure = Slope is shallow, may look similar to loop associated with increased R
AW
If you detect the patient actively working during mechanical breath, increase the flow to help meet the patient’s demand and decrease the WOB
To assess changes in compliance, use
Pressure vs Volume Loop
Steeper slope = increased compliance, or larger volume at lower pressure
Shallow slope = decreased compliance, or smaller volume at higher pressure
To assess changes in R
AW
, use
Pressure vs Volume Loop
Space – “hysteresis” – between inspiratory and expiratory portions of loop
“Bowed” appearance – inspiratory portion more rounded and distends toward the pressure axis
Flow vs Volume Loop
Observe peak flow on Flow-Volume Loop
Increased R
AW
= Decreased Peak Flow
UNIT B
Acute & Critical Care
PEEP/CPAP
PEEP – Positive End Expiratory Pressure
Definition
Application of pressure above atmospheric at the airway throughout expiration
Goal
To enhance tissue oxygenation
Maintain a PaO
2 above 60 mmHg with least amount of supplemental oxygen
Recruit alveoli
DECREASE (PA-a)02
Don’t forget (PA-a)02 will increase with v/q or shunt
HOW TO ACHIVE CPAP/PEEP
A. Exhaling through a spring tension diaphragm
B. Exhaling through a column of water
C. Exhaling through a partially inflated exhalation valve (mushroom type)
D. A continuous flow through the circuit
Indications
Cardiogenic pulmonary edema
Left sided heart failure
Prevents transudation of fluid
Improves gas exchange
ARDS
Increases lung compliance
Decreases intrapulmonary shunting
Increases FRC
Refractory hypoxemia
PaO
2
< 50 mmHg with an FIO
Increase FRC
2
Opens collapsed alveoli
Increases reserve
>50%
Contraindications
Unilateral lung disease
Hypovolemia
Hypotension
Untreated pneumothorax
Increased ICP
Hazards
All of the effects of CMV are magnified
Increased intrathoracic pressure
Decreased venous return
Increased ADH
Decreased blood pressure
Decreased cardiac output
Loss of thoracic pump
Barotrauma
Physiological effects
Baseline pressure increases
Increased intrapleural pressures
Increased FRC—recruiting collapsed alveoli
Dead space—increased in non-uniform lung disease and healthy lungs by distending alveoli
Increased alveolar volumes
Can increase compliance
Cardiovascular
Decrease venous return
Decrease cardiac output
Decrease blood pressure
Decreases intrapulmonary shunt
Increases mixed venous value (PvO
2 pulmonary artery via Swan-Ganz
)--Drawn from
Increased intracranial pressures
Decrease in A-a gradient (A-a DO
2
)
Increased PaO
2
Decrease in FIO
2
, which causes a decrease in PAO
2
I NITIATION AND MONITORING OF PEEP
Start off at 5 cmH
2 cmH
2
O increments
O and increase by 3 to 5
Adjust sensitivity
With an increase in baseline pressure the sensitivity must be increased or the patient will have to increase inspiratory effort to initiate a breath
Monitor
Blood pressure: First thing you look at when adding PEEP
Cardiac output: Goal is least cardiac embarrassment with the best PaO
2 and least FIO
2
Pulse
If the patient is hypoxemic their heart rate is probably increased
With addition of PEEP the hypoxemia should resolve and pulse should decrease to normal level
PaO
2
: Goal is best PaO
2
FIO
2 with the lowest possible
M AINTENANCE LEVEL OF PEEP
PEEP trial
Used to determine best level of PEEP
This is the pressure at which cardiac output and total lung compliance is maximized,the V
PaO
2 and PvO
2
D
/V
T is minimal, and the best
, and the lowest P(A-a)O
2 are obtained
Optimal Peep
Level at which physiological shunt (Qs/Qt) is lowest without detrimental drop in cardiac output
A C(
A-V
)O
2 of less than 3.5 vol% should reflect adequate CO
Fick’s law CO = VO
2
/C( a-v
)O
2
Cardiac output and C( a-v
)O
2 are inversely related
Best oxygenation with lease cardiac issues
CPAP
Physiologically the same as PEEP
Used in spontaneously breathing patients
Maintains continuous positive airway pressure during inspiration and expiration
Accomplished by a continuous flow of gas or a demand valve
System flow must be enough to meet patient’s peak inspiratory demands
Used to treat OSA
CPAP delivered via mask or nasal pillows
No machine breaths, all spontaneous ventilation
NPPV (B I PAP)
Similar to CPAP
Delivers two levels of pressure during the inspiratoryexpiratory cycle
Delivers higher pressure on inspiration
Delivers lower pressure on exhalation
Less resistance to exhalation
Two levels of pressure
EPAP
Constant pressure delivered during exhalation
Same as CPAP
Adjust for oxygenation
IPAP
Constant pressure delivered during inspiration
Same as IPPB
Adjust for ventilation
The difference between the two pressures is known as pressure support
Used to treat OSA
Better tolerated than traditional CPAP
Delivered with mask or nasal pillows
Used in acute respiratory failure
Can prevent or delay intubation and CMV
Improves ventilation and oxygenation
Improves patient comfort
R ULES OF PUTTING PATIENT ON PEEP
Obtain order
Set-up PEEP and make additional changes
(i.e., sensitivity)
Monitor patient for hazards, BP, CO if available
Monitor for "optimal/best PEEP"
60-60 Rule: to improve oxygenation increase fio2 to 60% then start adding peep (to prevent o2 toxicity). To remove peep go down to 60% and then start removing peep
IMV/SIMV
Definitions
IMV: Intermittent Mandatory Ventilation
Patient receives set number of mechanical breaths from the ventilator. In between those breaths, the patient can take their own spontaneous breaths at a rate and VT of their choice.
SIMV: Synchronized Intermittent Mandatory
Ventilation
Same as IMV, except the mechanical breaths are synchronized with the patient’s spontaneous respiratory rate. Helps improve patient/ventilator synchrony and helps prevent “breath stacking” (where the vent delivers the machine set VT on top of the patient’s spontaneous VT)
IMV
Advantages
Prevents muscle atrophy – makes patient assume an increasing, self-regulating role in their own respirations, helping to rebuild respiratory muscles
Allows patient to reach baseline ABGs – baseline means the patient’s baseline ABGs
Chronic CO of 40
2 retainer ABGs do not have a normal PaCO
2
Decreases mean intrathoracic pressure – the lower the
IMV/SIMV rate, the lower the intrathoracic pressure
Avoids decreased venous return – lower intrathoracic pressure = greater venous return
Avoids cardiac embarrassment – greater venous return = less decrease in cardiac output and blood pressure
May avoid positive fluid balance
Allows normalization of ADH production
Helps avoid cardiac embarrassment
Psychological encouragement
Some patients may exhibit anxiety, especially those who have been on the vent for several days or weeks
Do not tell the patient they will never need the vent again
Some patients become encouraged by progress, being able to do more for themselves
Weaning gradually – re-evaluate if weaning takes several days
May allow decreased use of pharmacological agents – e.g., morphine, diprivan, versed, etc.
If patient is too sedated, won’t be able to breathe spontaneously and participate in weaning
May be the only way to correct respiratory alkalosis on patient who is “over-breathing” the vent in A/C mode
Patient’s spontaneous V
T that of the set V
T will most likely be smaller than on mechanical ventilator
Candidates for IMV/SIMV
IMV/SIMV is great for weaning patient from CMV
Allows patient to assume increased responsibility for providing own respirations, with diminishing mechanical support
Allows patient to re-build respiratory muscle strength
Patient must be stable. Not ideal for unstable patient.
Consider patient unstable if
Fever – causes increased O2 consumption and increased
CO
2 production, thereby increasing WOB
Unstable cardiac status
Unresolved primary problem that caused them to be on the vent in the first place
Problems of IMV
Fighting the ventilator – patient becomes out of phase – or synch – with the ventilator
Stacking of breaths is not necessarily a problem
Patient will normally synchronize self with ventilator rate
Patient disconnection from gas source (with external IMV circuit)
Other problems of CMV
Benefits of SIMV – Synchronized IMV
Prevents stacking of breaths (pt can breath spontaneously through demand valve)
May help patient to become in phase with vent
Breath stacking could be prevented just by increase
inspiratory flow
I NSPIRATORY P RESSURE S UPPORT (IPS)
Commonly referred to simply as “Pressure
Support”
During spontaneous breathing, the ventilator functions as a constant pressure generator
Pressure develops rapidly in the ventilator system and remains at the set level until spontaneous inspiratory flow rates drop to 25% of the peak inspiratory flow (or specific flow rate)
This mode may be used
Independently
With CPAP
With SIMV
With any spontaneous ventilatory mode
Not with any full support modes, such as Control or A/C
PS is used to overcome the increased resistance of the ET tube and vent circuit
Pouiselle’s Law: decrease the diameter of a tube by ½, increase the resistance of flow through that tube by 16 times
If you apply/use PS, do not set less than 5 cmH
2
O of PS — least amount needed to overcome resistance of ET tube and vent circuit
If PS is set at a level higher than RAW, you will be adding to patient volumes, rather than just helping overcome the increased resistance from the ET tube and vent circuit
Can be used to help wean patient from vent and help rebuild respiratory muscle strength
M ANAGEMENT OF VENTILATORS BY ABG S
Pressure Control Ventilation
Can be used as CMV or SIMV
In SIMV mode, the machine breaths are delivered at the preset pressure while the spontaneous breaths are delivered with PS
PC-CMV (a.k.a., PCV) used to decrease shear forces that damage alveoli whenever the peak or plateau pressures meet or exceed 35cm H
2
O
Help prevent damage to alveoli from excessively high ventilating pressures
Shear forces damage alveoli when they collapse (because closing volumes are above FRC) and then are forced back open again with the next breath. Damage occurs as this cycle is repeated over time: alveoli collapses, then is reinflated, collapses, reinflated, etc.
Also used when permissive hypercapnia is desired (treatment of ARDS)
When the PaCO
2 is allowed to rise through a planned reduction in PPV, which allows for a reduction in the mean intrathoracic pressure, which results in less incidence of barotrauma and other commonly associated complications of PPV
The gradual increase in PaCO
2 is accomplished by a reduction of the mechanical VT (by decreasing the pressure) and usually does not affect the oxygenation
PC-IRV: Pressure Controlled Inverse Ratio
Ventilation
Pressure controlled ventilation with an I:E ratio > 1:1.
Causes mean airway pressure to rise with the I:E ratio
Usually used on patients with severe hypoxemia where high
F
I
O
2 s and PEEP have failed to improve oxygenation
Causes intrinsic PEEP (a.k.a. auto-PEEP), which is what causes the mean airway pressure to increase, which is the mechanism for alveolar recruitment and improved arterial oxygenation
While an increase in oxygenation does occur at the lung, a resultant decrease in cardiac output (due to the increased mean intrathoracic pressures) may result in an overall decrease in tissue oxygenation. Care must be exercised to maintain adequate cardiac output in order to maintain adequate tissue oxygenation
Because it’s not a natural way to breath (backwards from the way we normally breath), most patients must be either heavily sedated (Diprivan, Versed) or must be paralyzed with a paralytic drug (such as Pavulon or Norcuron)
APRV: Airway Pressure Release Ventilation
Related to PC-IRV except that patient breathes spontaneously throughout periods of raised and lowered airway pressure.
APRV intermittently decreases or releases the airway pressure from an upper CPAP (IPAP) level to a lower CPAP
(EPAP) level
The airway pressure release usually lasts 1.5 seconds or shorter, allowing the gas to passively leave the lungs to eliminate CO
2
I:E ratio is usually > 1:1, but differs from PC-IRV in that it allows spontaneous breathing
Because patient is breathing spontaneously, there is less need for sedation
Usually has lower peak airway pressure than PC-IRV
Originally proposed as a treatment for severe hypoxemia, but appears to be more useful in improving alveolar ventilation rather than oxygenation.
E ND T IDAL CO
2
M ONITORING (P
ET
CO
2
)
Measures CO
CO
2
2 level at end exhalation, when levels are highest in exhaled breath
Two methods of collection
Sidestream – typically used for non-intubated patients
Mainstream – typically used for intubated patients and more commonly seen and used
Probe is placed between the patient wye of vent tubing and the patient’s ETT
Infrared light measures CO
2 levels
Inspired gas should have value of zero
P
ET
CO
PaCO
2
2
content should be within 2 – 5 mmHg of patient’s
Difference will be greater on a patient with larger amounts of air trapping, e.g. Emphysema
C
APNOMETRY
(
CONT
.)
End-tidal CO
2
monitoring is for trending
Not absolute—can vary from breath to breath; similar to pulse oximetry
Look at the trend. Is the patient’s P
ET
CO
2 increasing or decreasing over a period of time? Similar activity should then be also occurring with the PaCO
2
When setup, correlate the P
ET
ABGs PaCO
2
P
ET
CO
2
CO
2 readings with current
. This will give you an idea of how much less the is reading than the PaCO
2
, giving you a good idea of future trends of the P
ET
CO
2 will relate to the PaCO
2
C HEST T UBE D RAINAGE S YSTEMS
Chest tube placed high in thoracic cavity to drain air
Second or third intercostal space at midclavicular line
Incision made right over the rib
Chest tube advanced towards anterior apex of lung.
Chest tube placed low in thoracic cavity to drain fluid (e.g., pleural effusion)
Placement is in fourth intercostal space (or lower) at midaxillary line
Patient is placed lying on side with affected side “up”
Once incision is made, tube is advanced posteriorly, toward the base of the lung so gravity can help drain the fluid
Three chamber chest tube drainage system is most common
Left chamber is the suction control chamber
Level of water determines how much suction is applied to the chest cavity, regardless of how much the suction is set on the suction regulator on the wall
Middle chamber is the water seal chamber
Usually no more than 2 cmH
2
O
Too much and you increase difficulty of air or fluid to drain
Too little and you risk an air leak
Bubbles in water seal indicate that a leak in the lung is still present
Spontaneous breathing patients with leak will have bubbles on exhalation
Intubated, mechanically ventilated patients with leak will have bubbles on inspiration
Continuous bubbling could be a sign of a leak in your chest tube drainage system and must be corrected immediately!
Clamp chest tube briefly where it exits patient’s chest. If bubbling stops, leak is in your patient (intrathoracic).
If bubbling persists, then you must check your chest tube drainage system for leaks
Move clamp down tubing in 10cm (approx. 4 inch) increments
(working from patient to chest tube drainage system), briefly clamping as you go until bubbling stops
Right chamber is the drainage collection chamber
This is where the fluid drained from the patient is collected
ALI=A CUTE LUNG INJURY OR ARDS
Definition agreed upon in 1994 at the American –
European Consensus Conference on ARDS
ALI Definition: a syndrome of acute and persistent lung inflammation with increased vascular permeability. Characterized by:
Bilateral radiographic infiltrates
A ratio PaO
2
/F
I
O
2 between 201 and 300 mmHg, regardless of the level of PEEP. The PaO
2 the F
I
O
2 is measured in mmHg and is expressed as a decimal between 0.21 and 1.00
No clinical evidence of an elevated left atrial pressure. If measured, the PCWP is 18 mmHg or less
ARDS Definition: same as ALI, except the hypoxia is worse. Requires a PaO
2
/F
I
O
2 ratio of
200 mmHg or less, regardless of the level of
PEEP. ARDS is ALI in its most extreme state
Mortality rate between 40 and 60%
-varies from source to source
Down from about 20 years ago when ARDS was almost certain death sentence with approximately 90% mortality rate.
Current Protective Lung Strategies
Lower V
T s with ALI/ARDS patients: about 6 ml/Kg IBW to avoid “volutrauma” from alveolar over distension
Sufficient PEEP to prevent alveolar collapse at end expiration, yet not so much that cardiac status is compromised
Permissive hypercapnia when treating
ALI/ARDS
PaO
2
> 65 mmHg
PIP < 35cm H
2
O
If your PIP is greater than 35cm H
2
O, consider using PCV
Closed suctioning system to maintain PEEP
Do not “bag” ALI/ARDS patient to “recruit more alveoli”; could lead to barotrauma or volutrauma
Monitor: Patient must be monitored closely as condition can change relatively quickly!
Things to monitor:
I&O
Cardiac output
BP
PIP
P
PLAT
Pulse Ox
F
I
O
2
V
T
V
E
CST
P
ET
CO
2
Waveforms
A-a Gradient
Renal vasoconstriction, due to hypoxemia, reduces urinary output.
Resolution of the hypoxemic state relieves the renal vasoconstriction, thus increasing urinary output.
M ANAGEMENT OF ABG S WITH CMV
ABG normal pH values
Normal range = 7.35 – 7.45
“Normal” = 7.40
PaCO
2
High PaCO
2 acidosis
Low PaCO
2 alkalosis will cause a low pH, thus causing respiratory will cause a high pH, thus causing respiratory
pH needs to be corrected so that drugs being given to patient will be metabolized
PaCO
2
and Ventilation
ABG normal PaCO
2 values
PaCO
2
/Ventilation = 35 – 45
“Normal” = 40
High PaCO
2 represents hypoventilation or the patient is under ventilated or retaining CO
2
Low PaCO
2 represents hyperventilation or the patient is over ventilated or blowing off CO
2
CO
2 represents how well your patient is ventilating. You would adjust V
T
, f, or remove dead space if on ventilator
PaCO
2
PaCO
2
& pH Calculations and pH have a direct relationship.
Starting at a PaCO
2
If PaCO
2 of 40 increases by 20 mmHg, pH decreases by 0.10
If PaCO
2 decreases by 10 mmHg, pH increases by 0.10
To increase PaCO
2
decrease VA
The PaCO
2
CO
2 is inversely proportional to VA providing that production remains constant
VA = (V
T
– V
D
)f
To decrease VA (increase PaCO
2
Decrease V
T
(keep in normal range)
)
Decrease f (will not blow off as much CO
2
)
Increase V
D bore tubing)
(only in control mode – 50cc per link of large
To decrease PaCO
2
VA = (V
T
– V
D
)f
increase VA
To increase VA (decrease PaCO
2
)
Increase V
T
(keep in normal range)
Increase f (will blow off more CO
2
)
Decrease V
D
Dead Space = Ventilation without perfusion
Anatomical dead space averages about 1 ml per pound
Alveolar dead space is alveoli that are ventilated but not perfused
Physiological dead space is the sum of the above
Normally, this is approximately 1/3 of the V
T
, or between
20 and 40% for spontaneously breathing, non-intubated patient
Normal for patient on ventilator is 40 – 60%
Formulas for V
D
/V
T
, Desired V
T
, & Desired f
V D /V T = PaCO2 – PetCO2
PaCO2
Gives the portion/percentage of V
T exchange.
not taking place in gas
S TRATEGIES TO ALTER VENTILATION
Always adjust V
T first, but remember to keep it in the normal range (8 – 12 ml/kg of ideal body weight)
If PaCO
2 is high, patient is on SIMV, and the patient is taking spontaneous breaths and the volumes are low, initiate Pressure Support to increase spontaneous volumes.
If you cannot adjust V
T the V
T up or down because it would place out of normal range, then change f (rate)
Change Mechanical Rate
Doing this alters Alveolar Ventilation
If your rate exceeds 20 bpm, auto-PEEP may develop
(patients with very stiff lungs. e.g., ARDS—may require higher f)
Increase f = decreased PaCO
2
Decrease f = increased PaCO
2
(hyperventilate)
(hypoventilate)
Add or remove V
Add V
DMech
DMech only in control mode to increase PaCO
2
Decrease V
DMech to decrease PaCO
2
Cut ETT to proper length to decrease dead space
Use low compliance vent circuit to decrease dead space
Large V
T and slow f are preferred to small V and rapid f because
T
Alveolar Ventilation is increased
Distribution of inspired gas is improved
Ventilation/Oxygenation is improved
Mean intrathoracic pressure is reduced
P A O
2
& O XYGENATION
PaO
2
/Oxygenation norm = 80 – 100
If PaO
2 is below 60, the patient has hypoxemia
For patients that are hypoxic and on a ventilator, adjust the F
2 to > 50% then start adding PEEP
I
O
When the patient improves, decrease F
I
O
2
40 – 50%, then start removing PEEP to prevent O
2 toxicity to
To increase PaO
2
(in any mode)
Increase F
I
O
2 if hypoxemia is caused by low
V/Q ratio to > 50%, then add PEEP to prevent oxygen toxicity. ( )
What is oxygen toxicity? How does it effect the patient?
When hypoxemia is present due to lung injury or physiological shunting (as in disease states like ARDS), add PEEP or CPAP
PaO
2 can be altered by either reducing or increasing PaCO levels by controlling VT
2
By reducing PaCO
2 levels (hyperventilation), PaO increase (RBCs can carry more O
2
)
2 levels
Works the opposite way, too—increasing PaCO
2 levels (hypoventilation), PaO2 levels decrease
(RBCs carry less O
2
)
T WO INDICES OF OXYGENATION
a/A Ratio
PaO
2
/PAO
2
O
2 from alveoli to blood
Divide PaO
2 by PAO
2
Normal = > 60%
A-a Gradient
P
(A-a)
O
2
Difference between alveolar and arterial PO
2
Also known as: - D(
A-a)
O
2
Subtract PaO
2 from PAO
2
Normal: - On 21%: 10 – 15 - On 100%: 65
On 100%, every 50 mmHg difference equals approx. 2% shunt
If under 300, you have V/Q mismatch so increase F i
O
2
If over 300, you have a shunt, so add PEEP or CPAP
First calculate PAO
2
Unless told otherwise
PBAR = 760
PH
2
O = 47
RQ = 0.8
(Pb-PH2O)fio2-(Paco2x1.25)
If F i
O
2 is greater than 60%, omit RQ from PAO2 formula
PaO
2 is obtained from an ABG
To decrease PaO
2
Decrease F
I
O
2
(in any mode)
Decrease PEEP gradually
If F
I
O
2
> 50% with PEEP, decrease F
(to reduce O
2 toxicity)
I
O
2 to 40 – 50% first
If patient remains stable and has an adequate PaO
2 to reduce PEEP slowly
, start
Increase PaCO
2
(Dalton’s Law)
Monitor patient at all times for signs of hypoxemia
M ANIPULATION OF ABG S IN CONTROL
MODE
To increase PaCO
2
Decrease V
T
Decrease f
Increase V
D
To decrease PaCO
2
Increase V
T
Increase f
Decrease V
D
M ANIPULATION OF ABG S IN A/C
To increase PaCO
2
Decrease VT: May be ineffective as pt. may increase f
Decrease f: Patient can increase assisting to override
Never add V
D in any mode but control
To decrease PaCO
2
Increase V
T
Increase f above assist rate
If ineffective, change to control or IMV modes
M ANIPULATION OF ABG S IN SIMV/IMV
To increase PaCO
2
Decrease V
T
– only to ranges for patient
Not best choice
Decrease f
Best choice towards weaning
Never add V
D in this mode
Will increase patient’s WOB and they will eventually fail
To decrease PaCO
Increase V
T
2
- stay within normal range
Increase f (blow off CO
2
)
Increase minute ventilation
May need to add PS to augment spontaneous volumes
Do not look at just the numbers and values
Always assess your patient with every ventilator change.
You are treating a patient, not a machine!