File
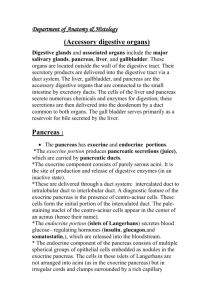
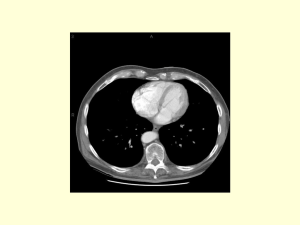
advertisement
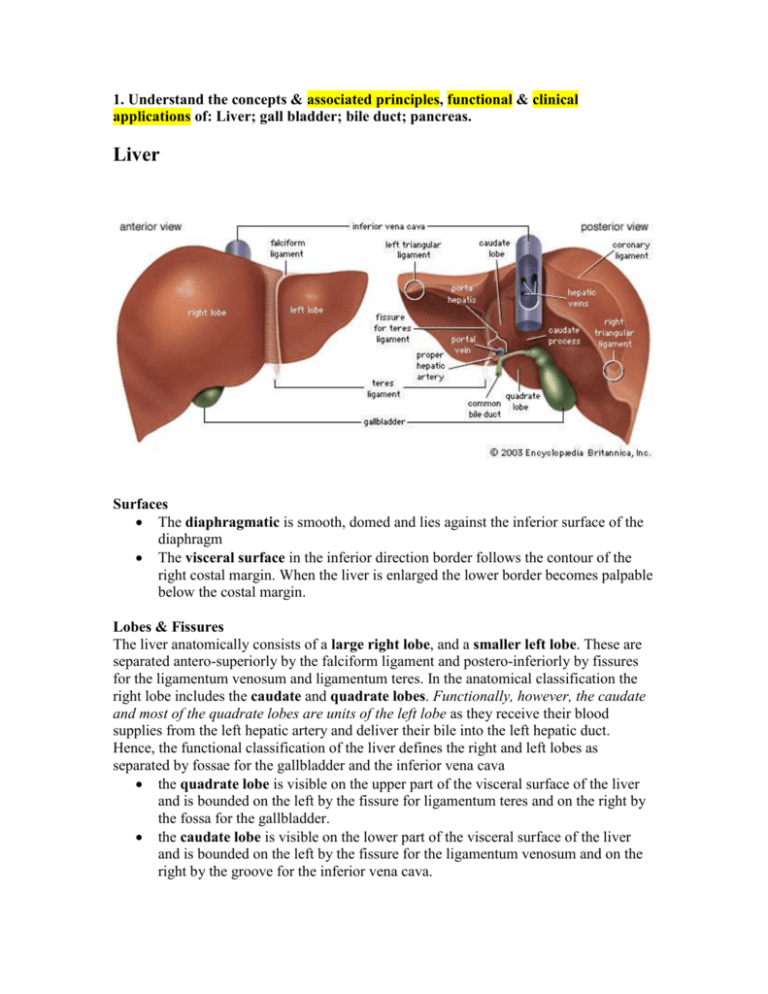
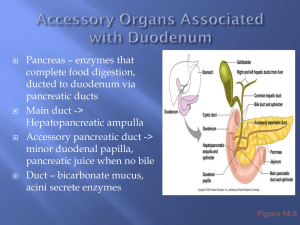
1. Understand the concepts & associated principles, functional & clinical applications of: Liver; gall bladder; bile duct; pancreas. Liver Surfaces The diaphragmatic is smooth, domed and lies against the inferior surface of the diaphragm The visceral surface in the inferior direction border follows the contour of the right costal margin. When the liver is enlarged the lower border becomes palpable below the costal margin. Lobes & Fissures The liver anatomically consists of a large right lobe, and a smaller left lobe. These are separated antero-superiorly by the falciform ligament and postero-inferiorly by fissures for the ligamentum venosum and ligamentum teres. In the anatomical classification the right lobe includes the caudate and quadrate lobes. Functionally, however, the caudate and most of the quadrate lobes are units of the left lobe as they receive their blood supplies from the left hepatic artery and deliver their bile into the left hepatic duct. Hence, the functional classification of the liver defines the right and left lobes as separated by fossae for the gallbladder and the inferior vena cava the quadrate lobe is visible on the upper part of the visceral surface of the liver and is bounded on the left by the fissure for ligamentum teres and on the right by the fossa for the gallbladder. the caudate lobe is visible on the lower part of the visceral surface of the liver and is bounded on the left by the fissure for the ligamentum venosum and on the right by the groove for the inferior vena cava. Porta Hepatis The porta hepatis serves as the point of entry into the liver for the hepatic arteries and the portal vein, and the exit point for the hepatic ducts Hepatic Ducts: Right and Left & Common The common hepatic duct is the combination of the right and left hepatic ducts in the porta hepatis. This structure courses, sequentially, in the free edge of the lesser omentum, behind the first part of the duodenum and in the groove between the second part of the duodenum and the head of the pancreas. It ultimately opens at the papilla on the medial aspect of the second part of the duodenum. Peritoneal attachments & Bare area The liver is attached to the anterior abdominal wall by the falciform ligament and, except for a small area of the liver against the diaphragm (the bare area), the liver is almost completely surrounded by visceral peritoneum. Additional folds of peritoneum connect the liver to the stomach (hepatogastric ligament), the duodenum (hepatoduodenal ligament), and the diaphragm (right and left triangular ligaments and anterior and posterior coronary ligaments). Blood Vessels The liver is made up of multiple functional units called lobules. Branches of the portal vein and hepatic artery transport blood through portal canals into a central vein by way of sinusoids which traverse the lobules. The central veins ultimately coalesce into the right, left and central hepatic veins which drain blood from corresponding liver areas backwards into the IVC. The extensive length of gut that is drained by the portal vein explains the predisposition for intestinal tumours to metastasize to the liver. Bile Production in the Bile Canaliculi within the Lobules The portal canals also contain tributaries of the hepatic ducts which serve to drain bile from the lobule down the biliary tree from where it can be concentrated in the gallbladder and eventually released into the duodenum. Gall bladder The gall-bladder lies adherent to the Visceral (undersurface) of the liver in the transpyloric plane at the junction of the right and quadrate lobes. The duodenum and the transverse colon are behind it. The gall-bladder acts as a reservoir for bile which it concentrates. It usually contains approximately 50 mL of bile which is released through the cystic and then common bile ducts into the duodenum in response to gall-bladder contraction induced by gut hormones. • Structure: the gall-bladder comprises a fundus, a body and a neck (which opens into the cystic duct). • Blood supply: the arterial supply to the gall-bladder is derived from two sources: the cystic artery which is usually, but not always, a branch of the right hepatic artery, and small branches of the hepatic arteries which pass via the fossa in which the gall-bladder lies. The cystic artery represents the most significant source of arterial supply. There is, however, no corresponding cystic vein but venous drainage occurs via small veins passing through the gall-bladder bed. Bile Duct The common hepatic duct is joined by the cystic duct to form the common bile duct. The common bile duct usually, but not always, joins with the main pancreatic duct Pancreas The pancreas has a: head, neck, body and tail. It is a retroperitoneal organ which lies roughly along the transpyloric plane. The head is bound laterally by the curved duodenum and the tail extends to the hilum of the spleen in the lienorenal ligament. The superior mesenteric vessels pass behind the pancreas, then anteriorly, over the uncinate process and third part of the duodenum into the root of the small bowel mesentery. The inferior vena cava, aorta, coeliac plexus, left kidney (and its vessels) and the left adrenal gland are posterior pancreatic relations. In addition, the portal vein is formed behind the pancreatic neck by the confluence of the splenic and superior mesenteric veins. The lesser sac and stomach are anterior pancreatic relations. • Structure: The pancreatic duct begins in the tail of the pancreas. It passes to the right through the body of the pancreas and, after entering the head of the pancreas, turns inferiorly. In the lower part of the head of pancreas, the pancreatic duct joins the bile duct. The joining of these two structures forms the hepatopancreatic ampulla (ampulla of Vater), which enters the descending part of the duodenum at the major duodenal papilla. Surrounding the ampulla is the sphincter of ampulla (sphincter of Oddi), which is a collection of smooth muscle. • Blood supply: the pancreatic head receives its supply from the superior and inferior pancreaticoduodenal arteries. The splenic artery courses along the upper border of the body of the pancreas which it supplies by means of a large branchathe arteria pancreatica magnaa and numerous smaller branches. • Function: the pancreas is a lobulated structure which performs both exocrine and endocrine functions. The exocrine secretory glands drain pancreatic juice into the pancreatic ducts and, from there, ultimately into the duodenum. The secretion is essential for the digestion and absorption of proteins, fats and carbohydrates. The endocrine pancreas is responsible for the production and secretion of glucagon and insulin, which take place in specialized cells of the islets of Langerhans. Exocrine Glands: A gland that secretes its products through a duct to the surface of the body or of an organ. The sweat glands in the skin and the salivary glands in the mouth are examples. The secretion is set off by a hormone (see HORMONES) or a NEUROTRANSMITTER. Endocrine Glands: Organs whose function it is to secrete into the blood or lymph, substances known as HORMONES. These play an important part in general changes to or the activities of other organs at a distance. Various diseases arise as the result of defects or excess in the internal secretions of the different glands.