Digestive System – Chapter 25
advertisement
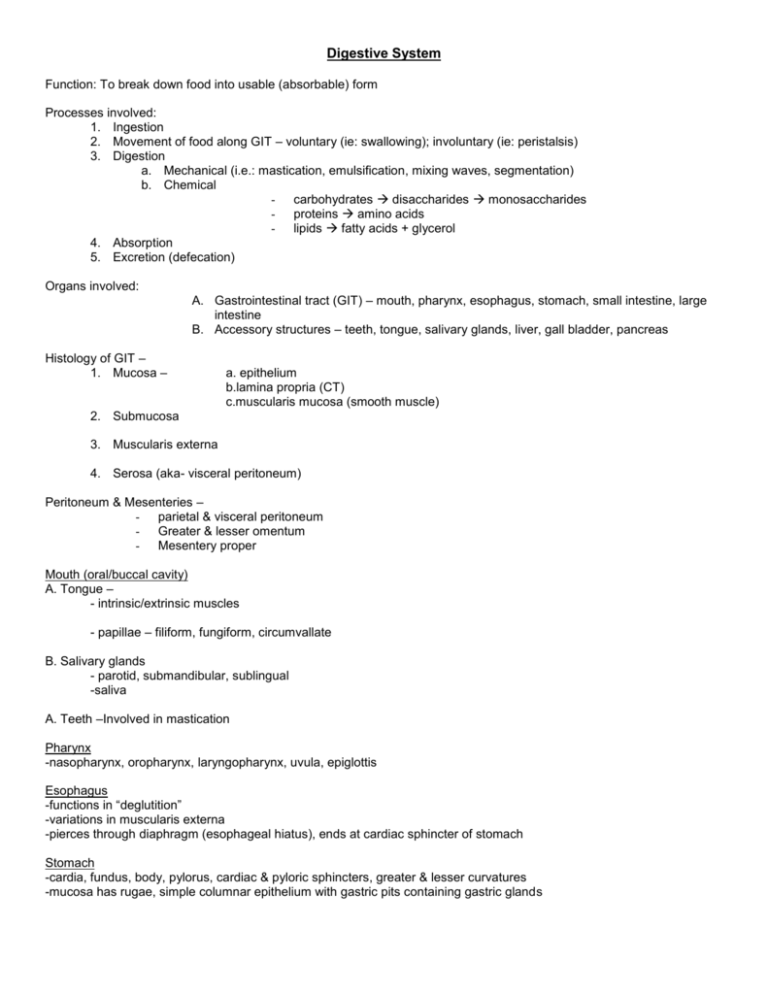
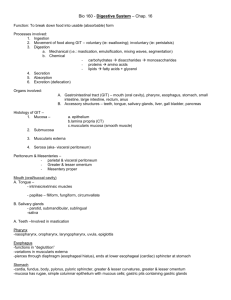
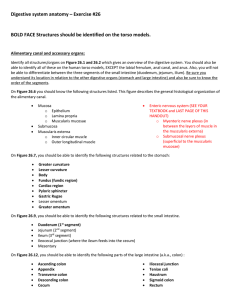
Digestive System Function: To break down food into usable (absorbable) form Processes involved: 1. Ingestion 2. Movement of food along GIT – voluntary (ie: swallowing); involuntary (ie: peristalsis) 3. Digestion a. Mechanical (i.e.: mastication, emulsification, mixing waves, segmentation) b. Chemical - carbohydrates disaccharides monosaccharides - proteins amino acids - lipids fatty acids + glycerol 4. Absorption 5. Excretion (defecation) Organs involved: A. Gastrointestinal tract (GIT) – mouth, pharynx, esophagus, stomach, small intestine, large intestine B. Accessory structures – teeth, tongue, salivary glands, liver, gall bladder, pancreas Histology of GIT – 1. Mucosa – a. epithelium b.lamina propria (CT) c.muscularis mucosa (smooth muscle) 2. Submucosa 3. Muscularis externa 4. Serosa (aka- visceral peritoneum) Peritoneum & Mesenteries – - parietal & visceral peritoneum - Greater & lesser omentum - Mesentery proper Mouth (oral/buccal cavity) A. Tongue – - intrinsic/extrinsic muscles - papillae – filiform, fungiform, circumvallate B. Salivary glands - parotid, submandibular, sublingual -saliva A. Teeth –Involved in mastication Pharynx -nasopharynx, oropharynx, laryngopharynx, uvula, epiglottis Esophagus -functions in “deglutition” -variations in muscularis externa -pierces through diaphragm (esophageal hiatus), ends at cardiac sphincter of stomach Stomach -cardia, fundus, body, pylorus, cardiac & pyloric sphincters, greater & lesser curvatures -mucosa has rugae, simple columnar epithelium with gastric pits containing gastric glands -gastric glands contain: a. peptic (chief) cells – secrete pepsinogen b. parietal cells- secrete HCL & intrinsic factor c. mucous cells – secrete mucous d. enteroendocrine (“G”) cells- secrete (among other things) gastrin -muscularis externa – 3 layers of smooth muscle (outer longitudinal/middle circular/inner oblique) -main function – protein digestion Small Intestine -1’’ diameter, 15-25’ long -duodenum -receives chyme from stomach, secretions from liver, gall bladder & pancreas -jejunum -most digestion & absorption occurs here -ileum – connects to large intestine at ileocecal sphincter/valve -modifications in mucosa & submucosa increase effectiveness of absorption: a. plicae circulares (circular folds) b. villi with capillary network and lacteal c. mucosal epithelium is simple columnar with microvilli (“absorptive cells”) and has intestinal crypts containing intestinal glands that secrete “intestinal juice” Pancreas -retroperitoneal -head (by duodenum), body, tail (by spleen) -endocrine (pancreatic islets of Langerhans) and exocrine gland (pancreatic acini) -“pancreatic juice” containing digestive enzymes ( amylase, trypsin, chymotrypsin, carboxypeptidase, lipase, nucleases) and bicarbonate secreted into pancreatic duct & released into duodenum Liver -2 main lobes (right & left) divided by “falciform ligament”, 2 smaller lobes –quadrate & caudate -lobes of liver divided into functional “lobules” containing rows of hepatic cells (“hepatocytes”) arranged radially around a “central vein”. Hepatocytes surround blood “sinusoids” which are partially lined by phagocytic “stellate reticuloendothelial (Kupffer) cells” -bile – produced by hepatocytes, secreted into bile canaliculi which merge to eventually form rt. & lt. Hepatic ducts which unite to form common hepatic duct which merges with cystic duct from gall bladder to form common bile duct which enters into duodenum -bile functions in “emulsification” of lipids, absorption of fats, and as an excretory substance -functions of liver include (but are not limited to): bile production & excretion, interconversion of nutrients, detoxification & removal of drugs, toxins & hormones from blood, storage of fat soluble vitamins & minerals, storage of glycogen, phagocytosis of worn out RBC’s, bacteria, & other pathogens -blood supply to liver – hepatic artery & hepatic portal vein into liver; hepatic veins from liver into IVC Gall bladder -stores & concentrates bile -cystic duct – merges with common hepatic duct to form common bile duct into duodenum Large Intestine -2-1/2 – 3” diameter, 5’ long -regions include: a. cecum – joined to ileum at iliececal sphincter, vermiform appendix b. colon – ascending transverse descending sigmoid c. rectum – becomes anal canal which opens at anus, internal & external anal sphincters -modifications in muscularis externa forming “taeniae coli” which create “haustra” -serosa forms “epiploic appendages” -main function – H2O reabsorption -no chemical digestion but some bacterial digestion -formation of feces for excretion Secretions of the GI Tract Organ Secretion Function Mouth (Salivary glands) Saliva (water, mucins, salivary amylase) Starch (polysaccharide) Maltose (disaccharide) Esophagus Mucus Lubrication 1. Peptic (Chief) cells Pepsinogen Proteins polypeptides 2. Parietal cells HCL intrinsic factor Converts pepsinogen pepsin, maintains acidic pH Vitamin B12 absorption 3. Mucous cells Mucus Protection 4. Enteroendocrine (“G” ) cells Gastrin (hormone) Stimulates secretion of gastric juice (pepsinogen, HCL, mucus); increases stomach motility Liver Bile (bile salts) Emulsification of fats, absorption of fatty acids & fat soluble vitamins (A,D,E,K) Pancreas Pancreatic amylase Starch (polysaccharide) maltose (disaccharide) Trypsin, chymotrypsin, carboxypeptidase Proteins & polypeptides smaller polypeptides & dipeptides Lipase Lipids (triglycerides) fatty acids + glycerol Nucleases Digests nucleic acids (RNA & DNA) Bicarbonate ions Neutralizes acidic chyme Disaccharidases (maltase, sucrase, lactase) Disaccharides monosaccharides (glucose, fructose, galactose) Peptidases Polypeptides dipeptides amino acids “Intestinal juice” Provides medium for absorption of nutrients Mucus Lubrication Stomach Small intestine Large intestine