Pressors - regionseminterns
advertisement

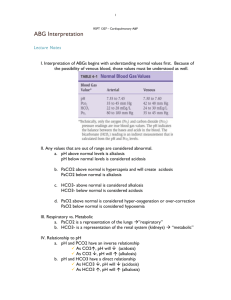
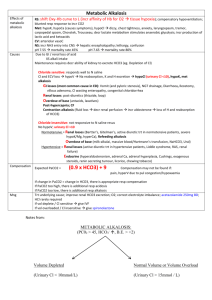
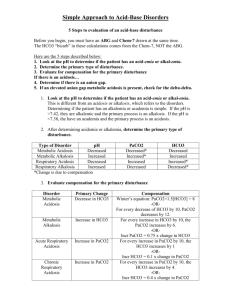
Drug Levophed (norepi) Receptors Alpha 1&2 > Beta 1 >>> Beta 2 Effects Vasoconstriction, increase SVR, minimal increase in HR Uses Shock, especially sepsis Dopamine (Low dose 0.5-2 mcg/kg/min) Dopaminergic (Low dose) Vasodilatation (Low dose) Renal dose (Mod dose 2-10 mcg/kg/min) Beta 1 >>> Beta 2 (Mod dose) Inotrope and chronotrope – increases HR, CO, contractility (Mod dose) Postop heart surgery (High dose >10 mcg/kg/min) Alpha 1 Alpha 1 (High dose) Vasoconstriction, increase SVR Vasoconstriction, increase SVR Vasopressin V1 and V2 Arterial vasoconstriction Epinepherine Alpha 1 & 2 (high dose = alpha > beta) Beta 1 & 2 Dobutamine Beta 1, Beta 2 >>> Alpha 1 High dose = alpha receptor vasoconstriction B1 = inotrope, increase HR/CO/contractility Minimal B2 effects. INOTROPE, NOT A PRESSOR Minimal alpha B1: Increases HR, CO, and contractility B2: Vasodilatation Positive intropic, vasodilating, and minimal chronotropic effects (despite B1). Neosynepherine Milrinone Isoproterenol Cyclic-AMP specific phosphodiesterase (PDE) inhibitor Beta 1 and 2 B1: Increases HR, CO, and contractility B2: Vasodilation Confirm the following: A – Airway established and secured B – Breathing adequate and work of breathing appropriate (sedation, analgesia, ventilation) C(a) – Circulation optimization – fluids, inotropes, pressors, ensure appropriately resuscitated (crystalloids). Pressors are ineffective without adequate volume. C(b) – Control O2 consumption – (sedation, fever, seizure control) D – Delivery of O2 adequate. (O2 sats, Hgb, lactate, SmVO2) – Consider fluids, transfusion, pressors, inotropes. E – Extraction of O2. Consider cyanide, met-Hgb, SEPSIS Adverse Effects Decreased tissue/organ perfusion. Must ensure pt has adequate intravascular volume. Arrythmogenic, prone to tachyarrythmias at higher doses (High dose) Shock 1) Head bleeds to maintain CPP goals 2) Neurogenic/spinal shock 3) To reverse hypotension with anesthesia Not titratable, either on or off. Adjunct to levophed, usually start when levo > 10. 1) Anaphylactic shock 2) CODES 3) All shock except cardiogenic Reflex bradycardia (due to no beta effects) 1) 2) 3) Hypotension if used as a pressor. 1) 2) 3) 1) 2) 3) Assist cardiac function CHF Adjunct in septic shock if cardiac dysfunction of sepsis is present Assist cardiac function CHF Adjunct in septic shock if cardiac dysfunction of sepsis present Assist cardiac function CHF Adjunct in septic shock if cardiac dysfunction of sepsis present Decrease gut perfusion, do not use in suspected mesenteric ischemia. LAST RESORT Avoid with cardiogenic shock as increases myocardial O2 demand. Most dysrhythmogenic Ventricular arrhythmia Electrolyte abnormalities Long half-life (1-2 hours) Angina, Adams-Stokes attacks, pulmonary edema, hypertension, hypotension, tachyarrhythmias (esp ventricular) Septic Shock 1) Check central venous O2 – less than 70% implies decreased DO2 and cardiac dysfunction of sepsis can be implied if: a. CVP 8-12 b. HCT >= 30% or Hgb >= 10 c. Lactate is normal (implying adequate resuscitation) 2) If CVO2 < 70%, may need inotrope. Start dobutamine in conjunction with pressor (Levophed). Titrate dobutamine to CVO2 sat > 70% and titrate Levophed to MAP affected by dobutamine. Ventilator Management (All kg-based calculations should be based on ideal body weight (IBW), not actual body weight, as lungs do not increase in size in relation to adipose tissue.) Typically start off with A/C volume control, rate 12-14, FiO2 100%, PEEP 5, tidal volume 8-10mL/kg. As you titrate, you should become uncomfortable with any rate > 22, PEEP > 15, or tidal volume > 10mL/kg. Ask for help. Your friendly respiratory therapists are an excellent resource in the absence of staff. Titrate down FiO2 to 30-40% if ABG’s show a reasonable pO2 and O2 sats are correlating. Don’t need to check an ABG after each change if O2 sats are reasonable. If pCO2 high or low, adjust rate and/or tidal volume. If pO2 high or low, adjust FiO2 and PEEP. Difficulty ventilating/oxygenating despite adjustments of rate, TV, FiO2, and PEEP (i.e. refractory low pO2, high peak/plateau pressures): Consider mucous plug, severe pneumonia (needs bronch?) PE??? Consider pressure control ventilation to manage peak/plateau pressures – accept whatever tidal volume you can get and adjust rate accordingly Consider starting nebulized Flolan – theoretically matches perfusion with ventilation by vasodilating vessels around alveoli which are being ventilated Consider rotating patient to prone position – re-distributes atelectasis and secretions to better ventilate healthy lung (???) Consider ultimate low-tidal-volume ventilation: THE OSCILLATOR!!! - Allows for oxygenation by diffusion, does not achieve ventilation so there is nothing you can do about pCO2. ARDS – low tidal volume ventilation – decrease tidal volumes to be no more than 6mL/kg, keep plateau pressures < 30mmHg. Ok to have higher pCO2 due to lower minute ventilations as long as pO2 is adequate (permissive hypercapnea). Adjust rate accordingly. Acute lung injury (ALL) = PaO2/FiO2 ratio of < 300 ARDS = PaO2/FiO2 ratio of < 200 ABG Interpretation A) Check internal consistency of ABG (is the test calibrated correctly, do the values make sense?) [H+] = 24 * (PaCO2 / [HCO3+] ) pH 7.10 7.20 7.30 7.40 7.50 7.60 [H+] 84 63 50 40 30 20 B) pH < 7.40 (Acidosis) a. pCO2 i. > 40 = primary respiratory acidosis 1. Acute (pH decrease by 0.08 for PaCO2 increase of 10mmHg) 2. Chronic (pH decrease by 0.03 for PaCO2 increase of 10mmHg) ii. < 40 1. Respiratory compensation for metabolic acidosis PaCO2 >= [HCO3+] * 1.5 + 8 [+ or – 2.0] 2. Concurrent respiratory alkalosis PaCO2 < [HCO3+] * 1.5 + 8 [+ or – 2.0] b. HCO3 i. < 24 1. Primary metabolic acidosis (if PaCO2 < 40) 2. Concurrent metabolic acidosis (if PaCO2 > 40) ii. > 24 1. Metabolic compensation HCO3 <= 24 + 0.4 * (PaCO2 – 40) 2. Concurrent metabolic alkalosis HCO3 > 24 + 0.4 * (PaCO2 – 40) C) pH > 7.40 (Alkalosis) a. pCO2 i. < 40 = Primary respiratory alkalosis ii. > 40 1. Respiratory compensation to metabolic alkalosis PaCO2 <= 40 + [0.7 * (HCO3 – 24) ] [+ or – 1.0] 2. Concurrent respiratory acidosis PaCO2 > 40 + [0.7 * (HCO3 – 24) ] [> + 1.0] b. HCO3 i. > 24 1. Primary metabolic alkalosis (if PaCO2 > 40) 2. Concurrent metabolic alkalosis (if PaCO2 < 40) ii. < 24 1. Metabolic compensation to respiratory alkalosis HCO3 >= 24 – 0.4 * (40 – PaCO2) 2. Concurrent metabolic acidosis HCO3 < 24 – 0.4 * (40 – PaCO2)