LOCAL ANAESTHETIC TOXICITY
advertisement

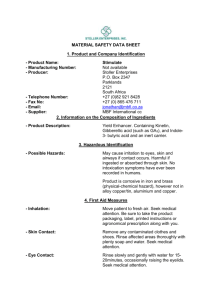
LOCAL ANAESTHETIC TOXICITY Higher Risk Bupivacaine Cocaine Lower Risk Prilocaine NB Contraindicated < 6 months age (from product info “may affect amount of oxygen in their blood) Doses: 1% is 1 g/100 mL Move decimal place to right (mg/ml) Ie 0.5% Prilocaine = 5mg/ml Adrenaline 1:1000 means 1 mg per 1 mL (ie, 0.1%) Amides Duration Doses Lignocaine (Xylocaine) Medium (30-60 min) Without epinephrine: 4.5 mg/kg; not to exceed 300 mg Lignocaine with epinephrine Long (120-360 min) With epinephrine: 7 mg/kg Bupivacaine (Marcaine) Long (120-240 min) Without epinephrine: 2.5 mg/kg; not to exceed 175 mg total dose Bupivacaine with epinephrine Long (180-420 min) With epinephrine: 3mg/kg Not to exceed 225 mg total dose Prilocaine (Citanest) Medium (30-90 min) Body weight <70 kg: 8 mg/kg; not to exceed 500 mg Body weight >70 kg: 600 mg OR: Biers: 3mg/kg, Plain 6mg/kg, +Adr 8mg/kg Comes in 0.5% = 250mg/50ml = 5mg/ml (hence “0.5ml/kg of 0.5%” for biers = 2.5mg/kg Ropivacaine (Naropin) Long (120-360 min) 5 mg/kg; not to exceed 200 mg for minor nerve block Reduced dosage is indicated in Debilitated or acutely ill Very young children Geriatric Liver disease Arteriosclerosis/Occlusive arterial disease NB: Topical doses can cause systemic toxicity, increased risk with abraded skin Cocaine containing preps have been assoc with seizures in kids Oral viscous lignocaine can cause toxicity with repeated doses Central nervous system signs Initial symptoms Lightheadedness Dizziness Blurred vision Tinnitus Disorientation/Drowsiness Higher-dose symptoms Initial CNS excitation followed by a rapid CNS depression Muscle twitching Convulsions Unconsciousness Coma Respiratory depression and arrest Cardiovascular depression and collapse Cardiovascular signs Direct cardiac effects Myocardial depression (tetracaine, etidocaine, bupivacaine), Cardiac dysrhythmias (bupivacaine) Several anesthetics also have negative inotropic effects on cardiac muscle that lead to hypotension. Bupivacaine is especially cardiotoxic. Peripheral effects Vasoconstriction at low doses Vasodilatation at higher doses (hypotension) The range of signs and symptoms of cardiovascular toxicity may include: Chest pain Shortness of breath Palpitations Lightheadedness Diaphoresis Hypotension Syncope Hematological signs Methemoglobinemia has been frequently reported in association with benzocaine use; however, lidocaine and prilocaine have also been implicated. O-toluidine, the liver metabolite of prilocaine, is a potent oxidizer of hemoglobin to methemoglobin. Low levels (1-3%), methemoglobinemia can be asymptomatic Higher levels (10-40%) may be accompanied by any of the following complaints: Cyanosis Cutaneous discoloration (gray) Tachypnea Dyspnea Exercise intolerance Fatigue Dizziness and syncope Weakness ALLERGY Amides are PABA derivatives associated with allergy Esters – no PABA but may contain preservative – methylparaben allergy Lignocaine allergy usually due to preservative Preservative-free ligocaine can be obtained Peripheral Neurotoxicity Persistent numbness from high doses Low pH and sodium bisulfite in the mixture can be partially responsible for these changes. Reversible skeletal muscle damage has also been reported TREATMENT OF TOXICITY 1) Allergy/anaphylaxis: usual treatment 2) Resuscitation& Stabilization of potential life threats. Ie Impending airway compromise, significant hypotension, and treatment of dysrhythmias and seizures. 3) CNS complications/toxicity = controversial No single remedy exists. Seizures: Benzodiazepines and barbiturates (eg, phenobarbital). Avoid phenytoin (shares pharmacologic properties ie, Na+ channel blockade with lidocaine may potentiate toxicity. 4) Cardiovascular: Prolonged PR, QRS, and QT intervals potentiating reentrant tachycardias with aberrant conduction may herald cardiovascular toxicity. Expect that cardiac resuscitation may be difficult and prolonged (30-45 min) Some anaesthetics = very lipid soluble require long time for redistribution. Most cases of lignocaine-induced cardiac toxicity can be successfully treated with properly CPR due to relatively short duration of action Avoid class IB antidysrhythmic agents (may worsen toxicity) Eg phenytoin, mexiletine (Mexitil), and tocainide (Tonocard) Bupivacaine depresses conduction and contractility at low doses. Lidocaine has been used successfully in bupivacaine-induced dysrhythmias, but its additive CNS toxicity is still a major concern. Even though bretylium theoretically should not potentiate CNS toxicity (as does lidocaine), its benefits in cardiovascular resuscitation are unclear. Evidence for use of amiodarone is also lacking Potential Options in prolonged/refractory resuscitation Adrenaline Vasopressin Cardiac pacing Bypass/ECMO Glucose/Insulin Lipid Emulsion Infusion (in Bupivicaine toxicity) Lipid Emulsion Infusion: Lipid infusion accelerates the decline in bupivacaine myocardial content (reduced tissue binding) by creating a lipid phase that extracts the lipid-soluble bupivacaine molecules from the aqueous plasma phase. A beneficial energetic-metabolic effect may also occur. To date, 3 successful case reports have been documented in humans. Weinberg's recommended dosing regimen for use in humans In cardiac arrest secondary to local anesthetic toxicity that is unresponsive to standard therapy, intravenous administration of a lipid such as Intralipid 20% is recommended in the following regimen: 1. Administer 1 mL/kg over 1 minute. 2. Repeat twice more at 3– to 5-minute intervals. 3. Then (or sooner if stability is restored), convert to an infusion at a rate of 0.25 mL/kg/min, continuing until hemodynamic stability is restored. 4. Increasing the dose beyond 8 mL/kg is unlikely to be useful. 5. In practice, resuscitate an adult weighing 70 kg as follows: 6. a. Use a 500-mL bag of fat emulsion (Intralipid 20%) and a 50-mL syringe. b. Draw up 50 mL and give it stat intravenously, and then draw up and give another 20 mL. c. Do exactly the same thing up to twice more as the epinephrine is given—if necessary or appropriate. d. Then, attach the fat emulsion bag to a giving set and administer it intravenously over the next 15 minutes. Note that propofol (Diprivan) is not a component of lipid rescue. It is formulated in a 10% lipid emulsion and therefore an overdose of propofol (gram quantities) would be necessary to provide an adequate dose of lipid emulsion. Propofol is contraindicated when there is any evidence of cardiovascular toxicity. Local Toxicity/nerve damage Local ischemic or nerve toxicities may occur, particularly in the extremities with prolonged anesthesia or epinephrine use. Suspected nerve damage should prompt neurologic consultation for urgent peripheral nerve studies. Vascular compromise Eg limb ischemia: consult a vascular surgeon immediately. Therapy for extravasation (eg, warm compresses, phentolamine, nitroglycerin cream) should be initiated for localized vascular toxicity. Methemoglobinemia Initially treat symptomatically and then guided by blood levels of methemoglobin. Methylene blue and hyperbaric oxygen may be required in severe cases. Finally, the prevention of local anesthetic toxicity should always be the primary consideration. Although all adverse reactions cannot be anticipated, complications can be avoided by strict adherence to the guidelines of anesthetic dosing, identification of patients at increased risk, and implementation of appropriate anesthetic application techniques to avoid unintentional intravascular injection.