INTRALIPIDS AS RESCUE
advertisement
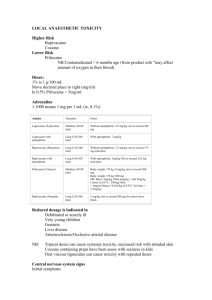
INTRALIPIDS AS RESCUE 2:30-3:30 Objectives • Describe signs and symptoms of local anesthetic (LA) toxicity. • Identify treatment modalities including use of lipids for patients with LA toxicity. • Identify factors influencing LA toxicity. Mechanism of action • Loss of sensation by – inhibiting excitation at nerve endings – blocking conduction in peripheral nerves • Progression of anesthesia related to affected nerve fiber: – diameter – myelination – conduction velocity • Prevent the development of action potential in nerve Regional Anesthesia • Involves the use of a local anesthetic strategically placed along the neural access to produce: – Surgical anesthesia – Postoperative analgesia – Analgesia for acute & chronic pain management • Goal: Block conduction of nociceptive (pain) impulses LOCAL AGENTS • Levels dependent on: – Dose – Rate of injection – Specific gravity of fluid – Position of patient LOCAL AGENTS • ESTERS Hydrolyzed in Plasma – Unstable in solution – Poor Penetrance – Fair to Poor Stability – • • • • • EXAMPLES Cocaine – (1884) Procaine - (Novacain) – 1984 Chloroprocaine (Nesacaine) Tetracaine(Pontocaine) - 1931 LOCAL AGENTS • AMIDES Metabolized by Liver – Stable Good Penetrance • Lidocaine - (Xylocaine) • Mepivacaine - (Carbocaine) • Prilocaine - (Citanest) • Bupivacaine - (Marcaine, Sensorcaine) • Etidocaine • Ropivacaine – LOCAL AGENTS • Epinepherine Added to Local – Vasoconstriction – Slows Vascular Absorption – Prolongs Effect Local Anesthesia Toxicity • Agents used in excessive doses or administered improperly. • Repetitive (small) doses to achieve an adequate level of anesthesia may lead to eventual administration of toxic dose. • Anesthesia injected into confined space • Doses may inadvertently be delivered as intravascular injection rather than epidurally Local Anesthesia Toxicity • Administration of toxic doses of LA – Increase disruptions of cellular metabolism – Interfere with inotropic function pathways that regulate NA+, K+ and Cl- ion flow – Modulation of autonomic system and enzymatic processes for ATP formation Toxicity • Early: agitation, lightheadedness, altered mental state, visual changes, slurred speech, hypertension and tachycardia • Middle: CNS excitation, cardiac dysrhythmias, contractile depression & conduction blockade. Seizure ( 20-30 minutes) • Severe: Hypotension, bradycardia, Ventricular dysrhythmia and cardiovascular collapse CNS Toxicity • • • • • • • • • • Sedation CNS excitation at low drug concentration Dizziness, ringing in the ear, Metallic taste Paresthesia (circumoral tingling) Anxiety Fear of death Uncontrolled muscle activity Tonic –clonic seizures CNS depression Bupivacaine ( CNS & Cardiac toxicity simultaneously Cardiovascular Toxicity • Block of sodium, calcium and potassium channels • Difficult to resuscitate on patient with asystole with Bupivacaine toxicity due to long term • Bupivacaine is cardiotoxic, strong attraction to myocardial sodium channel, slow dissociation from the sodium channels due to its lipophilic properties. Management of Local Anesthesia Toxicity • ACLS protocol – Airway – Vital Signs – Resuscitative Medications Chance Observation • Noted that patient with carnitine deficiency exhibited sensitivity to bupivacaine induced cardiac dysrhythnias, therefore postulated that bupivacaine might interfere with carnitine metabolism. • Carnitine = essential component of biochemical pathways that transport fatty acids into mitochondria where they provide the majority of cardiac energy needs. • Interestingly enough, the opposite was discovered – infusing lipids made them more resistant to bupivacaine-induced asystole. • Lipid infusion improves the success of resuscitation from bupivacaine toxicity. 2006 Case • 17 year old developed seizure activity and CV collapse after intentional ingestion. • Ingested: Bupropion (Antidepressant) and Lamotrigine (Anticonvulsant) • Unsuccessful resuscitation attempts for 70 minutes • 100 ml IV bolus of 20% lipid emulsion given • After 1 minute, an effective sustained pulse was observed. Patient recovered with no major neurologic deficit. 91 year old History: COPD, HTN, CAD, Reflux • Infraclavicular brachial plexus block for olecranon bursa excision. • Given 1% mepivicaine 30 ml • 20 min after injection was then injected with 10 ml 1% Prilocaine. • 5 minutes after injection of prilocaine, (20 min after patient received the Mepivicaine) patient developed dizziness, nausea, agitation & then lost consciousness • Given 1ml/kg bolus of 20% intralipid followed by infusion and patient recovered within minutes and surgery proceeded. 60 year old male with CAD, diabetes and end-stage renal disease • For Supraclavicular Brachial plexus block he received: – 30 ml 1.5% mepivacaine with bicarbonate and epi – 10 ml 0.5% bupivacaine • Developed labored respiration followed by obtundation 5 min after injection • CPR without re-establishment of effective cardiac rhythm • Given 20% lipid (250 ml over 30 min) patient recovered Local Anesthetic Systemic Toxicity (LAST) requiring treatment • 20 out of 10,000 peripheral nerve blocks • 4 out of 10,000 epidural blocks • Initial symptoms of LA Overdose – Mild hypertension – Tachycardia – Mild agitation – Confusion Cardiac Toxicity • • • • • Hypotension Atrioventricular conduction delay Idioventricular rhythms Respiratory depression Cardiovascular collapse Local Anesthetic Toxicity • Can occur after ingestion • IV administration • Topical Administration Checklist for Treatment of LAST (ASRA & Pain Medicine) • Get Help • Initial focus – Airway management – Seizure suppression ( Benzodiazepines NOT Propofol) – Alert nearest facility having Cardiopulmonary bypass capability • Manage cardiac dysrhymias – BLS & ACLS – Avoid Vasopressin, Calcium channel blockers, beta blockers and local anesthetics – Reduce epinepherine doses to <1mcg/kg Checklist for Treatment of LAST (ASRA & Pain Medicine) • Lipid emulsion therapy (20%) – – – – – Bolus 1.5 ml/kg IV over 1 minute Continuous infusion 0.25 ml/kg/min Repeat bolus once or twice for persistent CV collapse Double the infusion rate to 0.5 ml/kg/min if BP low Continue infusion for at least 10 min after attaining circulatory stability – Recommend upper limit: 10ml/kg/lipid emulsion over 30 min. • Post LAST events at www.lipidrescue.org or www.lipidregistry.org Lipid Sink • Expanded plasma lipid compartment that traps lipophilic drugs • Infused intravascular lipid mass binds the offending toxin in sufficient quantity to pull drug from the target tissue, thereby reversing the toxicity. • Successful resuscitation suggest the efficacy of lipid emulsion infusion for treating non-local anesthetic overdoses across a wide spectrum of drugs: beta blockers, calcium channel blockers, parasiticides, herbicides and several varieties of psychotropic agents. 2 Proposed methods of How Intralipids Work • 1. Lipid infusion creates a lipid phase in the plasma to which local anesthetics partition into. • 2. Reversal of mitochondrial fatty acid transport inhibition – Believed LA inhibit carnitine acylcarnitine translocase (CACT) – an enzyme used in mitochrondrial fatty acid metabolism and transport – Because fatty acids are involved in 80-90% of cardiac adenosine 5-triphosphate (ATP) synthesis, inhibition of CACT may contribute to cardiac toxicity. – Lipid infusion may increase the intracellular fatty acid content enough to overcome the inhibition of the CACT enzyme by the anesthetic. Death of woman at a Laser Treatment Center • Patient received cream containing 10% Lidocaine and 10% Tetracaine. • Patient applied cream over Large areas of skin then wrapped her legs in cellophane which increased the absorption of the drug. • Found seizing in her car. • Unable to resuscitate Lipid Therapy Side Effect • Allergic reaction, headache, somnolence, dizziness, dyspnea, diaphoresis, N&V, hyperthermia and hypercoagulability • Thrombocytopenia, jaundice, overloading syndrome, Increased liver function, leucopenia, hepatomegaly, splenomegaly • Pulmonary hypertension with long term therapy • Yeast infection Conclusions • Lipid infusion appears to reverse cardiotoxicity rapidly and is easier than cardiopulmonary bypass. • Lipid emulsion is readily available at a much lower cost. • Lipid rescue therapy is to be reserved until ACLS procedures have been unsuccessful in cases of local anesthetic toxicity Summary • Nurses plan an important role towards a successful outcome for patients with local anesthesia toxicity • Know your high risk patients • Recognize signs and symptoms of toxicity • Have adequate emergency equipment available when resuscitation needs arise • Know your facility policy for Local Anesthesia Toxicity