Pharmacology Case #6
advertisement
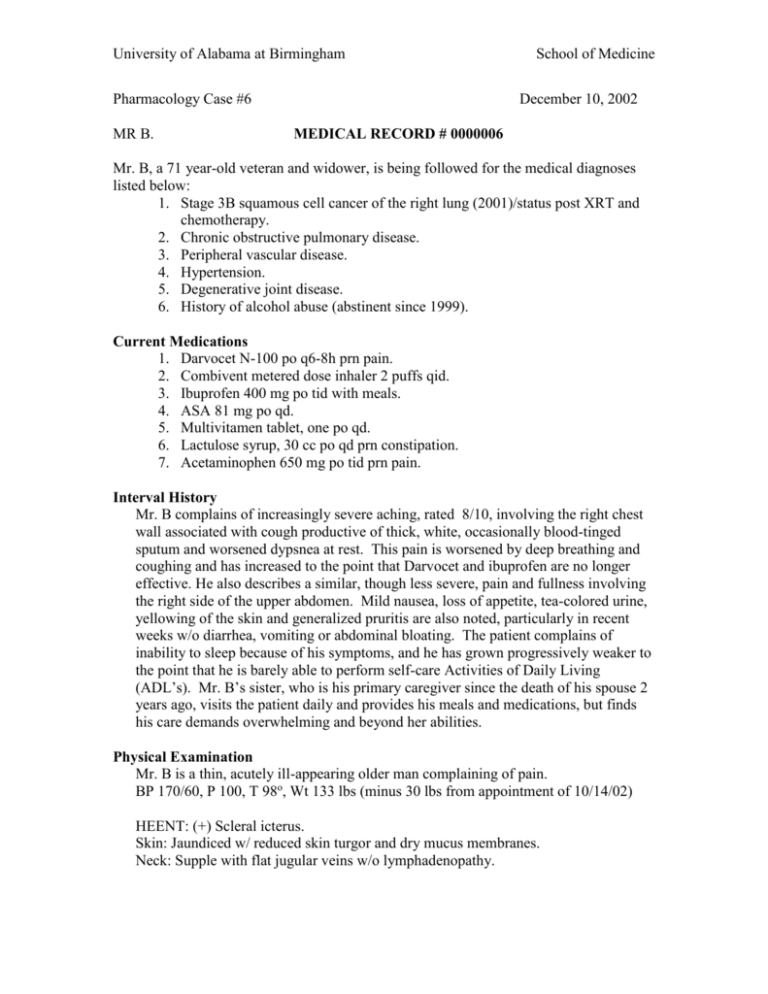
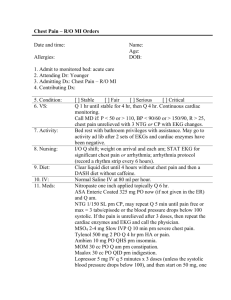
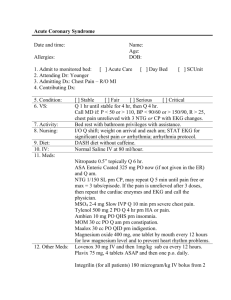
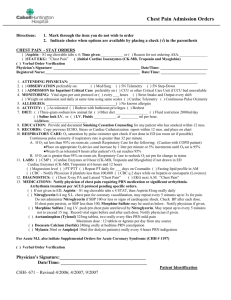
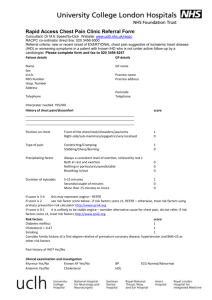
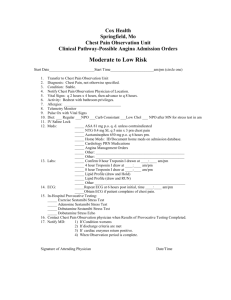
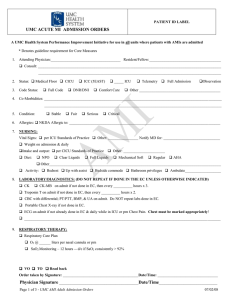
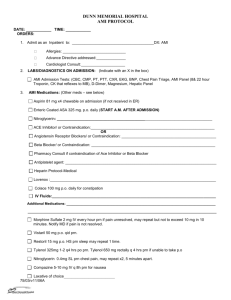
University of Alabama at Birmingham Pharmacology Case #6 MR B. School of Medicine December 10, 2002 MEDICAL RECORD # 0000006 Mr. B, a 71 year-old veteran and widower, is being followed for the medical diagnoses listed below: 1. Stage 3B squamous cell cancer of the right lung (2001)/status post XRT and chemotherapy. 2. Chronic obstructive pulmonary disease. 3. Peripheral vascular disease. 4. Hypertension. 5. Degenerative joint disease. 6. History of alcohol abuse (abstinent since 1999). Current Medications 1. Darvocet N-100 po q6-8h prn pain. 2. Combivent metered dose inhaler 2 puffs qid. 3. Ibuprofen 400 mg po tid with meals. 4. ASA 81 mg po qd. 5. Multivitamen tablet, one po qd. 6. Lactulose syrup, 30 cc po qd prn constipation. 7. Acetaminophen 650 mg po tid prn pain. Interval History Mr. B complains of increasingly severe aching, rated 8/10, involving the right chest wall associated with cough productive of thick, white, occasionally blood-tinged sputum and worsened dypsnea at rest. This pain is worsened by deep breathing and coughing and has increased to the point that Darvocet and ibuprofen are no longer effective. He also describes a similar, though less severe, pain and fullness involving the right side of the upper abdomen. Mild nausea, loss of appetite, tea-colored urine, yellowing of the skin and generalized pruritis are also noted, particularly in recent weeks w/o diarrhea, vomiting or abdominal bloating. The patient complains of inability to sleep because of his symptoms, and he has grown progressively weaker to the point that he is barely able to perform self-care Activities of Daily Living (ADL’s). Mr. B’s sister, who is his primary caregiver since the death of his spouse 2 years ago, visits the patient daily and provides his meals and medications, but finds his care demands overwhelming and beyond her abilities. Physical Examination Mr. B is a thin, acutely ill-appearing older man complaining of pain. BP 170/60, P 100, T 98o, Wt 133 lbs (minus 30 lbs from appointment of 10/14/02) HEENT: (+) Scleral icterus. Skin: Jaundiced w/ reduced skin turgor and dry mucus membranes. Neck: Supple with flat jugular veins w/o lymphadenopathy. University of Alabama at Birmingham School of Medicine Chest: Increased AP diameter with decreased breath sounds throughout. Dull w/ increased fremitus, bronchial breath sounds and e-to-a changes in the right anterior hemithorax. Heart: Point of maximum impulse not palpable with an increased S1 and a physiologically split S2 w/o murmurs or gallops Abdomen: Soft, protuberant with normoactive bowel sounds. Liver is firm, tender and 18 cm in span w/ an irregular, nodular edge 5 fingerbreadths beneath the right costal margin. W/o splenomegaly, shifting dullness, guarding. Extremities: Trace edema at the ankles w/o clubbing or cyanosis. Absent pedal pulses. Neurological: W/o asterixis. Laboratory Chemistry panel: Na 147, K 3.4, Cl 110, CO2 38, Glu 100, BUN/crea 8/0.9. CBC: Hct/hgb 30%/10.2, wbc 11, plts 140,000. LFT’s: Alk phos 438, SGOT 225, SGPT 199, LDH 400, total bilirubin 4.4, direct bilirubin 3.0, albumin 3.4. Right upper quadrant abdominal ultrasonogram: Numerous nodules, consistent with metastases, are noted in an irregularly enlarged liver. Nondilated intra- and extra-hepatic bile ducts are seen, as is a normal-appearing spleen, gallbladder and pancreas. Chest radiograph (AP and lateral views): An enlarging lung mass abutting the mediastinum and involving the right middle lobe and the chest wall is seen. Boney lesions of the adjacent ribs, most likely due to direct spread of tumor, are appreciated. Enlarged ipsilateral and contralateral mediastinal lymph nodes are noted. The chest x-ray is otherwise remarkable for changes consistent with COPD and a normal cardiac silhouette. Supported by a grant from the Association of American Medical Colleges and the John A. Hartford Foundation.