Documentation ECA Temple College
advertisement
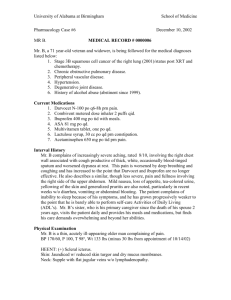
Documentation ECA Temple College Purpose of Documentation Patient Care The most important reason Record for other health care providers to reference at a later date Becomes part of patient record for later use Legal Record May be used in court proceedings May be your sole source of reference Other Uses Medical Audit Quality Improvement Evaluate and improve individual performance Evaluate and improve system quality Billing and administration Run Review Conferences Other Educational Forums Gather data necessary for economic and regulatory purposes Research Studies to improve patient care and system performance Types of written reports Traditional written form with check boxes and a section for narrative. Computerized version where information is filled in by means of an electronic clipboard or a similar device. Did you know information “missing” in your prehospital report may prove more valuable to an attorney than the information that is actually written in the report…. “The missing Protocol” Sections of a report Run Data Patient Data Narrative Run Data Date Times Name of service Unit number Names of crew members Patient Data Patient name Address Date of birth Insurance information Sex Age Nature of call or mechanism of injury Patient Data Location of patient Treatment administered prior to arrival of ECA Signs and symptoms Care administered by first responders Baseline vital signs SAMPLE history Changes in condition. Issues of Credibility Misspelled words Illegible handwriting Poor writing skills Added information well after the event… USE OF ABBREVIATIONS USE ONLY AUTHORIZED MEDICALLY RECOGNIZED ABBREVIATIONS DO NOT MAKE UP YOUR “OWN” ABBREVIATIONS. Narrative Styles SOAP CHARTE Body Systems Chronological SOAP(E) Subjective Objective Analysis (or Assessment) Plan Enroute (or changes) Liquid SOAPE Subjective Also called the history of the present illness/injury. Contains the patient’s symptoms or complaints. In the patient’s own words, but skillfully condensed. Formally, contains the past medical history, current medications and allergies. Objective Also called the physical examination. Contains your observations (signs). Formally, contains the vital signs. Avoid subjective terms: normal, poor, good, or WNL. Analysis Also called the clinical impression or presumptive diagnosis. It is a summary of the objective and subjective sections. It is not a formal diagnosis Often includes a triage category. Plan The actual plan and delivery of patient care. Not what you wished you had done. Rescue before resuscitation, resuscitation before definitive treatments. Sometimes responses to treatment are listed. Enroute Also called changes or response to treatment (especially by non-transporting first responders). Narrative Written account of what occurred. Include information that is not included in other sections of the report. Be Objective The patient was drunk. VS The patient had slurred speech, smelled of alcohol, was not able to make coordinated movements, and admitted to drinking alcohol. Allow reader to draw the desired Patient Information Minimum information gathered at time of ECA's initial contact with patient on arrival at scene, following all interventions and on transfer of care or arrival at facility. Chief complaint Level of consciousness (AVPU) - mental status Systolic blood pressure for patients greater than 3 years old Skin perfusion (capillary refill) for patients less than 6 years old Skin color and temperature Pulse rate Respiratory rate and effort For every reassessment, record time and findings. Patient Care Errors You are human, you will make mistakes. Learn from them and do not make them again Be honest and forthcoming about your error Falsification Issues Error of omission or commission occurs Falsification of information Do not try to cover it up. Document what did or did not happen What steps were taken (if any) to correct the situation. Suspension or revocations of certification Removal of ability to practice in system Specific areas of difficulty Vital signs - document only the vital signs that were actually taken. Treatment - if a treatment like oxygen was overlooked, do not chart that the patient was given oxygen. Correction of Written Errors Errors discovered while the report form is being written Draw a single horizontal line through the error, initial it and write the correct information beside it. Do not try to obliterate the error - this may be interpreted as an attempt to cover up a mistake. Errors discovered after the report form is submitted Preferably in a different color ink, draw a single line through the error, initial and date it and add a note with the correct information. If information was omitted, add a note with the correct information, the date and the EMT-Basic's initials. Correction Examples During writing Mr. Smith complains of shortness of breath, chest pain, and jaw arm pain After completed Mr. Smith complains for jaw pain. JDF, 10/12/06 Addendum: Mr. Smith complained of arm pain not jaw pain. This was discovered after reviewing the original report. This addendum is intended to correct this error. Jeff Fritz 10/13/2006 11:20 am Patient Refusal Competent adult patients have the right to determine what does and does not occur to their body Thus they have the right to refuse all or part of the care you offer. Refusals Perform a complete and detailed assessment Ensure the patient is able to make a rational, informed decision, e.g., not under the influence of alcohol or other drugs, or illness/injury effects. Inform the patient What is wrong with the patient (from detail assessment) Why he should go to the hospital (what care can they provide) What may happen to him if he does not (consequences) Alternatives to transport and or treatment Consult medical direction as directed by local protocol. Try again to persuade the patient to go to a hospital. Before you leave the scene If the patient still refuses, document any assessment findings and emergency medical care given, then have the patient sign a refusal form Have a family member, police officer or bystander sign the form as a witness. If the patient refuses to sign the refusal form, have a family member, police officer or bystander sign the form verifying that the patient refused to sign. Inform patient of your willingness to return Document the Refusal Your assessment findings What you told the patient What is wrong, why he should go, consequences, alternatives, and your willingness to return. The patient understood all of the above What the patients comments were Your attempts to convince the patient to go Mass Casualty Incidents The local MCI plan should have some means of recording important medical information temporarily, e.g., triage tag, that can be used later to complete the form. The standard for completing the form in an MCI is not the same as for a typical call. The local plan should have guidelines. Written Report When information of a sensitive nature is documented, note the source of that information, e.g., communicable diseases. Be sure to spell words correctly, especially medical words. If you do not know how to spell it, find out or use another word. Include pertinent negatives. If you expect to find something and it is not there i.e. patient with chest pain who is not short of breath Written Report Confidentiality – the form itself and the information on the form are considered confidential. Only those with a need to know should see it Billing Other health care providers who will care for patient This does not include other members of your organization Common Errors Misspelled words Poor grammar Illegible handwriting Unknown or improper abbreviations Incomplete forms Examples pateint CP, TD, PERRLA patient were bedridden patient complains of laceration thigh pain Report Example Subjective: 59 year old male complaining of substernal chest pain that radiates to left arm and jaw. Onset around 15:30 after argument with son. Pain not improved or relieved with position or breathing changes. Pain is described as dull pressure and rated at 8/10. Pt also complains of SOB and weakness. Pt denies nausea, vomiting, dizziness. History: HTN. Allergies: NKDA. Medications: Procardia 30mg/day. Objective: Pt sitting in chair in obvious pain. Pt’s fist rubbing chest. Mental Status: Awake, responds appropriate to questions Skin: cool, diaphoretic. HEENT: 0 wounds, PEARL, No accessory muscle use, + JVD, Bruits present. CHEST: 0 wounds, bilateral basilar rales, non tender, no discoloration. ABD: soft, non tender, no masses, no wounds. PELVIS: deferred. EXT: moves all extremities, + pulse, +sensory, Flow chart time 1602 1604 1610 1615 1618 1619 MS awake -------- -------- -------- -------- -----> 132/60 130/p 128/p BP 112 118 104 HR 22 24 22 RR MS, ASA meds meds stretcher trans arrival Assessment: MI – Urgent Plan: Oxygen via NRB @ 15 lpm, vital signs, ASA 324 mg PO, nitroglycerin 0.4 mg SL, repeat vital signs, prepare for transport, verbal report given to M. Smith. Pt transported with M12