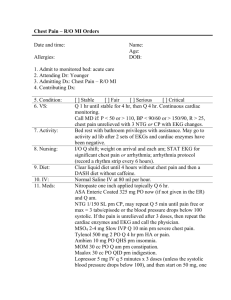
Chest Pain – R/O MI Orders
advertisement
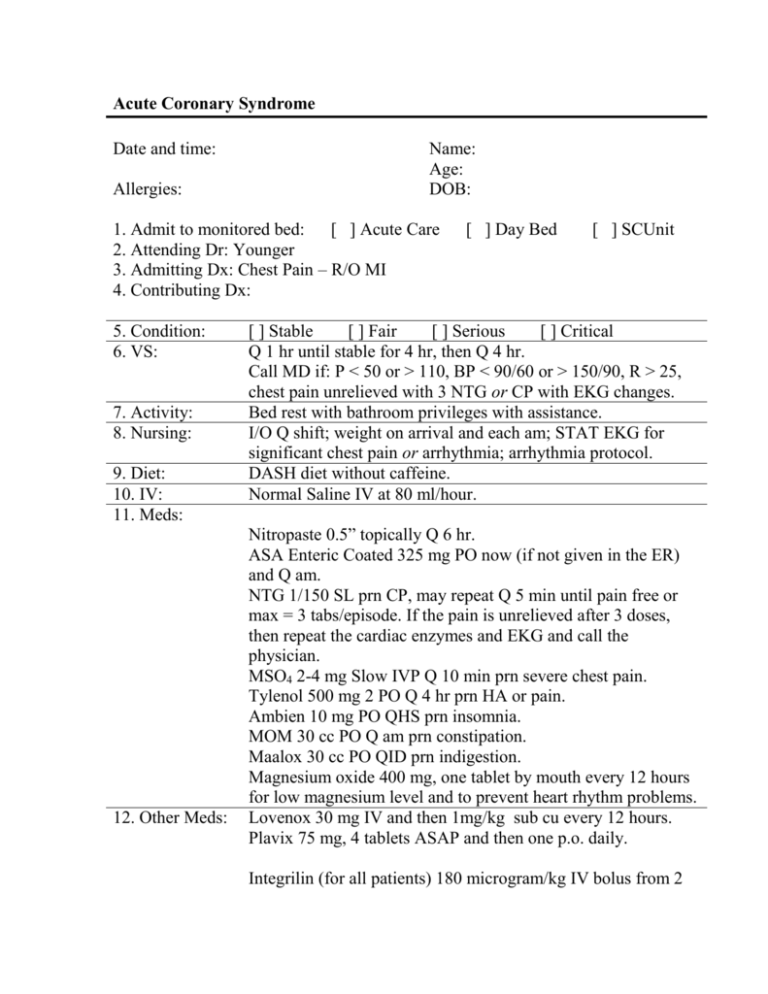
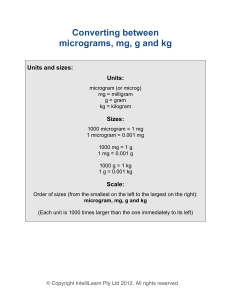
Acute Coronary Syndrome Date and time: Allergies: Name: Age: DOB: 1. Admit to monitored bed: [ ] Acute Care 2. Attending Dr: Younger 3. Admitting Dx: Chest Pain – R/O MI 4. Contributing Dx: 5. Condition: 6. VS: 7. Activity: 8. Nursing: 9. Diet: 10. IV: 11. Meds: 12. Other Meds: [ ] Day Bed [ ] SCUnit [ ] Stable [ ] Fair [ ] Serious [ ] Critical Q 1 hr until stable for 4 hr, then Q 4 hr. Call MD if: P < 50 or > 110, BP < 90/60 or > 150/90, R > 25, chest pain unrelieved with 3 NTG or CP with EKG changes. Bed rest with bathroom privileges with assistance. I/O Q shift; weight on arrival and each am; STAT EKG for significant chest pain or arrhythmia; arrhythmia protocol. DASH diet without caffeine. Normal Saline IV at 80 ml/hour. Nitropaste 0.5” topically Q 6 hr. ASA Enteric Coated 325 mg PO now (if not given in the ER) and Q am. NTG 1/150 SL prn CP, may repeat Q 5 min until pain free or max = 3 tabs/episode. If the pain is unrelieved after 3 doses, then repeat the cardiac enzymes and EKG and call the physician. MSO4 2-4 mg Slow IVP Q 10 min prn severe chest pain. Tylenol 500 mg 2 PO Q 4 hr prn HA or pain. Ambien 10 mg PO QHS prn insomnia. MOM 30 cc PO Q am prn constipation. Maalox 30 cc PO QID prn indigestion. Magnesium oxide 400 mg, one tablet by mouth every 12 hours for low magnesium level and to prevent heart rhythm problems. Lovenox 30 mg IV and then 1mg/kg sub cu every 12 hours. Plavix 75 mg, 4 tablets ASAP and then one p.o. daily. Integrilin (for all patients) 180 microgram/kg IV bolus from 2 microgram/ml vial. For normal renal function (serum creatinine < 2.0), follow the bolus with an infusion of 2.0 microgram/kg/min from 0.75 mg/ml, 100 ml vial. For decreased renal function (serum creatinine between 2.0 and 4.0), follow the bolus with 1.0 microgram/kg/min from 0.75 mg/ml, 100 ml vial. Continue infusion until hospital discharge, for up to 72 hours, or until transfer of the patient for coronary intervention surgery. 13. Respiratory therapy: 14. Consultants: 15. Labs: Oxygen at 2 liters per minute by nasal cannula (maintain SpO2 level > 92%) for 12 hours after the last chest pain. Recheck a SpO2 level after removal of the O2 to ensure the SpO2 is > 90%. If it is < than 90%, then reapply oxygen to maintain a SpO2 level > 90% and daily try to retitrate the oxygen requirements of the patient on room air. Total CK, monoclonal CK-MB, troponin I on admission (if not done in ER) and 8 hr later for total of 3. Call if abnormal. CBC, if not done in ER. Chem 8, magnesium, and LFTs, if not done in ER. Lipid profile fasting in am. CXR (portable) if not done in ER. EKG on admission (if not done in ER) and with each cardiac enzyme panel. ________________________________________________ Signature