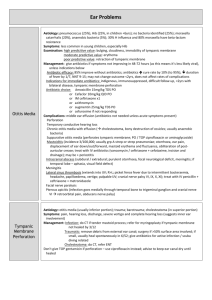
OTITIS EXTERNA PREVENTION Advise patients to refrain from
advertisement
OTITIS EXTERNA PREVENTION Advise patients to refrain from excessive manipulation or cleaning of the external ear canal. Discuss with parents the naturally bacteriostatic environment of the ear canal and the risks of instrumentation, particularly with cotton swabs. Advise patients to prevent or reduce excess moisture in the ear canal. Consider advising patients, especially in humid climates, to either avoid water sports or to consider the use of drying agents (primarily alcohol-based agents) only when repeated, significant episodes of external otitis are a problem. Note that protective devices such as ear plugs are necessary only in patients with recurrent episodes DIAGNOSIS Consider the diagnosis of otitis externa in patients with otalgia, ear discharge, or pruritus and pain on manipulation of the auricle. Ask about: Water exposure History of trauma or manipulation Diabetes mellitus Immunocompromised state Dermatitis of the external auditory canal Otalgia, or pain with chewing Ear discharge Ear fullness Pruritus Hearing loss (conductive) Examine the ear for evidence of infection localized to external auditory canal. Look for: Erythema Edema Discharge (may be scant) Exfoliated skin or squamous debris Thickened epithelium or “cobblestone” appearance of the skin Interruption of the tympanic membrane or the presence of tympanostomy tubes DIAGNOSTIC TESTS Consider microbiologic and/or radiologic studies in patients presenting with unusual symptoms and signs and in those who are refractory to prior treatment. Note that no lab or radiographic tests are needed at outset and treatment is initiated based on clinical findings. Perform microbiological tests to identify the organism and appropriate therapy in persistent otitis externa. Perform radiologic studies such as CT of the temporal bone with evidence of bone cancer or MRI of the head in patients with unusual symptoms and signs such as severe headache, vertigo, or nystagmus, or in patients with refractory otitis externa symptoms who are immunocompromised or have diabetes mellitus. Consider other infectious, inflammatory, or neoplastic processes involving the skin, soft tissue, cartilage, or bone surrounding the auditory canal. Be aware that any dermatologic disorder can potentially manifest itself in the ear. Recognize that otitis externa can encompass a broad spectrum of disease processes ranging from local bacterial infections such as furunculosis to invasive, potentially systemic MOE(malignant otitis externa) Consider other diagnoses when otitis externa fails to resolve with appropriate therapy or when specific history or findings suggest a more likely diagnosis. CONSULTATION Consider consulting an otolaryngologist if clinical findings suggest complex or atypical disease. Consider consulting an otolaryngologist when the diagnosis is unclear based on unusual history or findings on physical exam, such as: TM perforation Exposed bone Abundant granulation tissue Cholesteatoma Significant canal wall erosion Consider consultation for management in all patients who require extensive management beyond ototopical antibiotics. Refer to an otolaryngologist: When refractory otorrhea prevents adequate visualization of the tympanic membrane For aggressive aural toilet using suction debridement under microscope or for wick placement For surgical management including incision and drainage or debridement HOSPITALIZATION Hospitalize patients when systemic or significant local complications of otitis externa such as cellulitis are present. Hospitalize patients with fever or evidence of cellulitis beyond the ear canal for antibiotic therapy. THERAPY Relieve obstruction of the ear canal. Under direct vision with otoscope, carefully apply a cerumen wire, cotton-tipped swab, or unraveled cotton ball to the external canal to promote removal of debris and otorrhea as needed. Consider referral to otolaryngologist for suction debridement under microscopic visualization when initial standard therapy fails. Use ototopical agents as first-line treatment of uncomplicated otitis externa. Use topical agents as first-line therapy for uncomplicated disease. Consider: Acetic acid with or without hydrocortisone Ciprofloxacin with or without a corticosteroid (More rapid relief of symptoms than topical antibiotics alone) Ofloxacin Neomycin (Ototoxicity with neomycin if used with tympanic membrane perforation or if used longterm), polymyxin, and hydrocortisone Use quinolone in patients with tympanostomy tubes or perforated tympanic membranes. Treat with oral or intravenous antibiotics only in patients whose infection has spread beyond the ear canal. Use systemic antibiotics if infection has spread beyond the external canal. Consider systemic antibiotics in patients who are at increased risk for complications, including those with uncontrolled diabetes or who are immunocompromised. Treat pain in patients with otitis externa. Treat pain in patients with otitis externa. Note that pain may be severe. Consider treatment with: An oral NSAID or acetaminophen A topical steroid An opioid in patients with severe pain Select the form of topical therapy based on patient factors. Maximize therapeutic benefit by choosing an appropriate drug form and delivery mechanism. Consider ototopical spray before drops for superior patient tolerance and clinical response. Advise patients to restore and maintain normal ear physiology. Advise patients to avoid water exposure and instrumentation of ear. Consider acidifying drops to reduce pH and inhibit bacterial growth. Consider desiccating solutions for residual moisture, as persistent moisture may lead to prolongation of infection and potential for fungal overgrowth. PATIENT COUNSELLING Inform patients with otitis externa about clinical course, importance of adherence to therapy, potential complications, and secondary prevention. Advise patients: To use drops for 7 to 10 days or longer depending on physician recommendations To keep follow-up appointments for debridement to aid in drop delivery and time to cure That most cases of external otitis resolve within 7 to 10 days That follow-up is important to ensure resolution of disease and to allow the clinician to eliminate other diagnoses in cases of persistent disease FOLLOW UP Follow the patient until resolution of disease is confirmed. Schedule follow-up: As frequently as every other day or at least once a week to ensure resolution of disease To remove debris and facilitate drop placement To confirm appropriate response to therapy as persistent disease may require further work-up to investigate alternative diagnoses Refer patients with nonresponsive or recurrent disease to a specialist for suction debridement under the operative microscope, wick placement, or examination for other underlying disease. Elements of Follow-up for Otitis Externa