Otitis Externa
advertisement

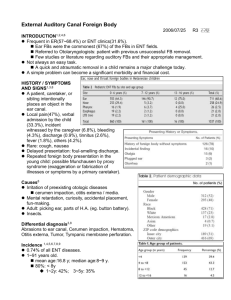
Four Interesting Topics for the Veterinary Practitioner Otitis externa, Otitis media, Craniomandibular Osteopathy and Equine Wobblers Syndrome By : Anabel Holt, AVC 2011 http://www.petergray.org.uk/pictures/horse1.jpg http://www.askspikeonline.com/wp-content/uploads/2009/02/adult-westie1.jpg Otitis Externa Acute or chronic inflammation of the external ear canal more commonly seen in dogs than cats • • Common causes include parasites, hypersensitivity reactions, foreign bodies, obstructions, and autoimmune diseases Perpetuating factors include, but are not limited to, bacterial overgrowth/ infections, yeast overgrowth/ infections, canal hypertrophy, cerumen gland hyperplasia and adenitis http://www.marvistavet.com/assets/images/ear_canal.gif Pre-disposing Factors • • • Otitis externa is more commonly seen in humid environments, and in the summer months associated with atopy. Idiopathic Glandular Hyperplasia of Cocker Spaniels, Springer Spaniels, excessive hair in the ear canals (Cocker Spaniels and Poodles), pendulous pinnae , and stenotic ear canals (ex: Shar Peis). Dogs that swim a lot in the summer months often have a greater risk http://www.petwellbeingblog.com/uploaded_images/ear-infection-751033.jpg Clinical Signs Associated with Otitis Externa • • Head shaking, rubbing, scratching, discharge from the external ear canal, aural erythema, alopecia of the ear pinnae, hyperplasia of the ear canal wall, hearing deficits and possibily generalized skin disease Chronic/End Stage Otitis externa: Calcification of auricular cartilage The Different Types of Aural Discharge and their Causes: Brown “coffee ground” like discharge: ear mites Brown or Gay discharge: Malassezia (yeast) Yellow-white discharge: Ceruminous Yellow-green discharge: Bacteria Name this ectoparasite. http://www.google.ca/imgres?imgurl Otodectes cynotis How do you diagnose Otitis Externa? • History, clinical signs, physical exam findings, cytologic examination, +/- bacterial culture and sensitivity When should a culture and sensitivity analysis be done on an ear swab? When ROD shaped bacteria are present! http://www.avianbiotech.com/Diseases/Images/salmonella.jpg What do you see radiographically? • • Stenosis with an increase in soft tissue opacity in the external ear canal, and in end stage cases, mineralization of the canal The VD view is best The Atlantic Veterinary College, PEI Treatment Options • • • • • • Topical or Systemic corticosteroids Antibiotics - repeat cytology every two weeks to determine if treatment is working and whether changes need to be made Antifungal drugs Ear flushing Resolution often takes up to 3-4 weeks (for the treatment of mites) Treatment for chronic otitis externa with end stage obstruction: Total ear canal ablation Bullae osteotomy Otitis Media • • • • An infection of the middle ear, most commonly as the result of the extension of otitis externa through a ruptured tympanum Bacteria (primary agents), yeast, neoplasia and nasopharyngeal polyps are common causes Other causes may include mites (predispose animal to bacterial infections), trauma, and foreign bodies Neoplasia and nasopharyngeal polyps are a common causes of refractory otitis media What diagnostic procedure should be done in all chronic/reoccurring otitis externa cases? An otoscopic exam! Clinical Signs • • • • • • • • The patient may have a head tilt towards the affected ear. The animal may paw at the affected ear. Often a resting or positional rotary or horizontal nystagmus is present An ipsilateral ventral strabismus may be seen Ipsilateral mandibular lymphadenopathy may be present On otoscopic examination, the tympanic membrane may appear dull, bulging and opaque Pain may be observed when opening the mouth Facial nerve damage and Horner’s syndrome may be seen What does it look like radiographically? • • • The opacity of the tympanic bullae is increased Thickening of the bullae walls are seen (they should be “egg shell” thin) Best visualized with obliques or open mouth rostrocaudal views http://www.vin.com/AppUtil/Image/handler.ashx?imgid=556937&w=300 Treatment • • • • • • • • • 2-4 month course of systemic antibiotics to prevent relapse (resolution often takes six or more weeks) Antifungals Corticosteroids (anti-inflammatory dosage) Consider flushing ear (s) under general anesthesia Recheck in 10-14 days Vestibular signs (head tilt, nystagmus etc), often improve within 2-6 weeks Owner should be warned that the head tilt and any facial nerve damage or Horner’s Syndrome may remain Surgical treatment (save for unresponsive or relapsing infection) Bullae osteotomy - complications may include Horner’s Syndrome, Facial paralysis, Vestibular dysfunction, and deafness • Ear ablation through horizontal ear canal Craniomandibular Osteopathy (CMO) • • • • • A nonneoplastic, non-inflammatory proliferative disease involving the bones of the head Usually bilaterally symmetrical Commonly affected breeds include Scottish Terriers, Cairn Terriers, Boston Terriers and West Highland Terriers Commonly affected bones: Mandibular rami, occipital and parietal bones, tympanic bullae, zygomatic portion of the temporal bone Affects the musculoskeletal system - particularly the muscles involved with prehension and mastication http://www.google.ca/imgres?imgurl CMO • • • • • Most likely hereditary basis: autosomal recessive in Westies Usually affects puppies 4-8 months of age Mandibular swelling, irregular thickening of mandibular rami/ TMJ region Temporal and masseter muscle atrophy is common Difficulty/pain with chewing, self-limiting pyrexia http://www.marvistavet.com/assets/images/dog_chewing_muscles.gif What does CMO look like radiographically? • Bony proliferation on affected bones (mandibular rami, occipital and parietal bones, tympanic bullae, zygomatic portion of temporal bone) http://dvminsight.com/ImageLibrary/JPGViewer/JPGViewer.aspx?DEXAM=103551&IMAGENAME=IMAGE_0001.jpg Differential DDX for CMO • Osteomyelitis • Traumatic periostitis • Neoplasia http://content.answers.com/main/content/img/elsevier/vet/gr91.jpg Treatment Options • • • • Primarily palliative May diminish at skeletal maturity (10-12 months of age) Often surgical placement of a feeding tube and a high calorie, protein rich gruel diet needed Do not breed affected animals, or repeat breeding of dam and sire http://www.google.ca/imgres?imgurl=http://vetneuromuscular.ucsd.edu Crossing to the Other Side: Equine Wobblers Syndrome • 1. • 2. • Two Main types: Cervical Vertebral Instability (ages 2 months-2 yrs) A dynamic stenosis found commonly at C5-C6, C6-C7, that compresses the spinal cord when the neck is flexed. Cervical Static Stenosis (5-10 yrs of age) A narrowing of the vertebral canal , most often at C3-C4, C5-C6, that persists as the neck is put in different ranges of motion *Affected horses are often noted as fast growing, and of a large frame http:/ / www.equinewobblers.com/ Surgery/ Surgery.htm Clinical Signs •Slowly progressive ataxia and weakness of the limbs, with the hind limbs more affected •Signs may appear acutely or worsen after trauma •UMN/LMN signs are seen •Knuckling of the fetlocks, toe dragging, tripod stance, circumduction of hind limbs when circled tightly, reluctance to back, proprioceptive deficits, weak sway response, OCD and DJD are often seen in conjunction with these syndromes (vertebrae, articular facets, multiple joints) Differential Diagnoses 1. Cervical Fractures 2. Equine Protozoal Myeloencephalitis 3. Equine Degenerative Myeloencephalopathy 4. EVH-1 5. Intervertebral Disk Protrusion 6. Space Occupying Mass Diagnostics http://www.equinewobblers.com/Diagnostics/Standing-cervical_radiographs.htm • • 1. 2. • • Radiographs Tentative Diagnosis: Narrowing of the cervical canal, DJD of the facet joints, malalignment of vertebrae (evidence of malalignment include: metaphyseal and epiphyseal flaring, uneven lengths of the vertebral body and dorsal lamina, malformation and OCD of the articular facets) Must be lateral Can measure stenosis: Measure width of the cranial vertebral orifice and of the widest portion of the epiphysis of the cranial vertebral body. Divide the width of the orifice by the width of the body Normal ratios: C2-C6: greater than 0.56, C7: greater than 0.58 ratios less than this indicate stenosis Diagnostics continued… •Myelography- best diagnostic procedure to confirm the diagnosis •General anesthesia is needed •Special Skills •High energy x-ray machine http://www.equinewobblers.com/Diagnostics/Myelogram.htm Treatment Options 1. Conservative (stall rest, hand walking, altered diet etc) 2. Surgery: Ventral Cervical Vertebral Stabilization 3. Dorsal decompressive laminectomy (replaced by Ventral Cervical Vertebral Stabilization). http://rammfence.files.wordpress.com/2010/01/horse-in-stall-46cropped-e1263228993887.jpg Questions? http://www.hnsa.org/doc/pt/know/img/pg2.jpg References • • • • Brown, M., Christopher & Joseph J. Bertone (2001). The 5- Minute Veterinary Consult Equine. Lippincott Williams & Wilkins, PA. Cote, Etienne (2007). Clinical Veterinary Advisor Dogs and Cats. Mosby Elsevier, Missouri. Stashak, S. Ted (2002). Adams’ Lameness In Horses (5th ed.). Lippincott Williams & Wilkins, PA. Tilley P. L. & Francis W.K. Smith Jr. (2007). Blackwell’s Five-Minute Veterinary Consult: Canine & Feline (4th ed). Blackwell Publishing, Iowa.