Ear Problems
advertisement
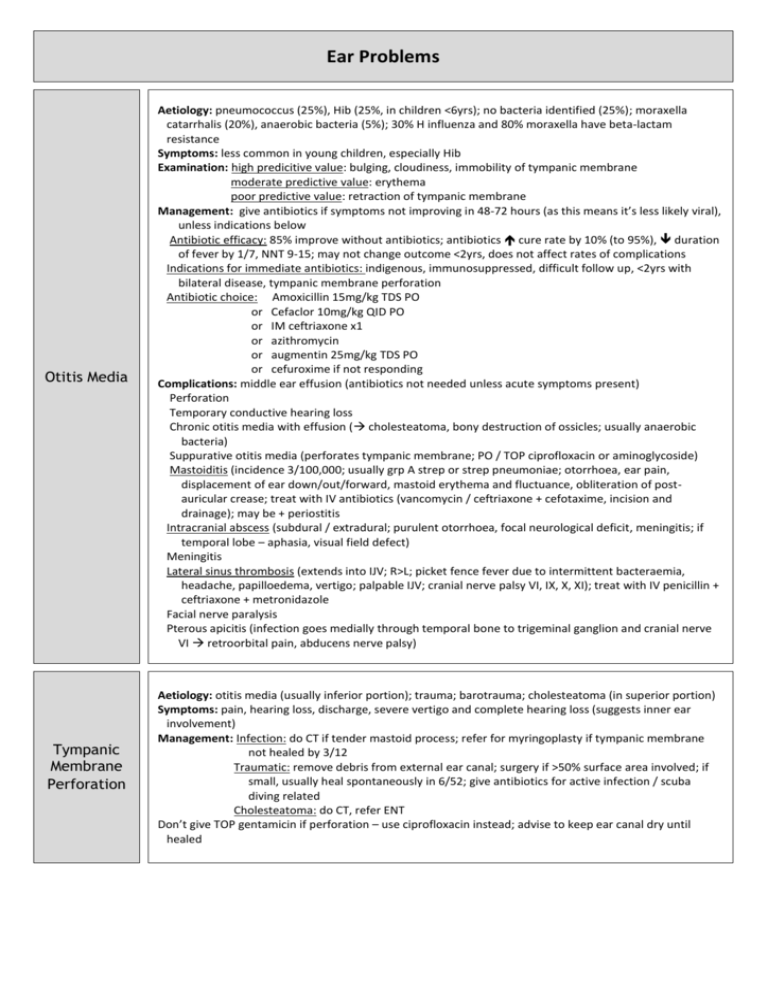
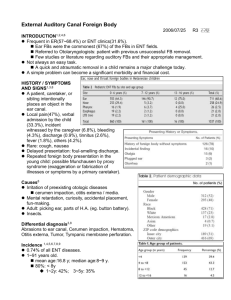
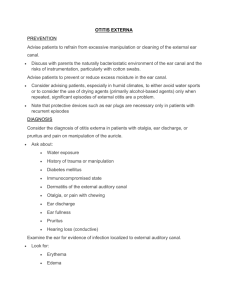
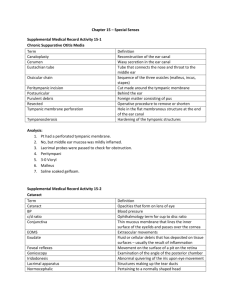
Ear Problems Otitis Media Aetiology: pneumococcus (25%), Hib (25%, in children <6yrs); no bacteria identified (25%); moraxella catarrhalis (20%), anaerobic bacteria (5%); 30% H influenza and 80% moraxella have beta-lactam resistance Symptoms: less common in young children, especially Hib Examination: high predicitive value: bulging, cloudiness, immobility of tympanic membrane moderate predictive value: erythema poor predictive value: retraction of tympanic membrane Management: give antibiotics if symptoms not improving in 48-72 hours (as this means it’s less likely viral), unless indications below Antibiotic efficacy: 85% improve without antibiotics; antibiotics cure rate by 10% (to 95%), duration of fever by 1/7, NNT 9-15; may not change outcome <2yrs, does not affect rates of complications Indications for immediate antibiotics: indigenous, immunosuppressed, difficult follow up, <2yrs with bilateral disease, tympanic membrane perforation Antibiotic choice: Amoxicillin 15mg/kg TDS PO or Cefaclor 10mg/kg QID PO or IM ceftriaxone x1 or azithromycin or augmentin 25mg/kg TDS PO or cefuroxime if not responding Complications: middle ear effusion (antibiotics not needed unless acute symptoms present) Perforation Temporary conductive hearing loss Chronic otitis media with effusion ( cholesteatoma, bony destruction of ossicles; usually anaerobic bacteria) Suppurative otitis media (perforates tympanic membrane; PO / TOP ciprofloxacin or aminoglycoside) Mastoiditis (incidence 3/100,000; usually grp A strep or strep pneumoniae; otorrhoea, ear pain, displacement of ear down/out/forward, mastoid erythema and fluctuance, obliteration of postauricular crease; treat with IV antibiotics (vancomycin / ceftriaxone + cefotaxime, incision and drainage); may be + periostitis Intracranial abscess (subdural / extradural; purulent otorrhoea, focal neurological deficit, meningitis; if temporal lobe – aphasia, visual field defect) Meningitis Lateral sinus thrombosis (extends into IJV; R>L; picket fence fever due to intermittent bacteraemia, headache, papilloedema, vertigo; palpable IJV; cranial nerve palsy VI, IX, X, XI); treat with IV penicillin + ceftriaxone + metronidazole Facial nerve paralysis Pterous apicitis (infection goes medially through temporal bone to trigeminal ganglion and cranial nerve VI retroorbital pain, abducens nerve palsy) Tympanic Membrane Perforation Aetiology: otitis media (usually inferior portion); trauma; barotrauma; cholesteatoma (in superior portion) Symptoms: pain, hearing loss, discharge, severe vertigo and complete hearing loss (suggests inner ear involvement) Management: Infection: do CT if tender mastoid process; refer for myringoplasty if tympanic membrane not healed by 3/12 Traumatic: remove debris from external ear canal; surgery if >50% surface area involved; if small, usually heal spontaneously in 6/52; give antibiotics for active infection / scuba diving related Cholesteatoma: do CT, refer ENT Don’t give TOP gentamicin if perforation – use ciprofloxacin instead; advise to keep ear canal dry until healed Otitis Externa Epidemiology: most common ear infection in adults Aetiology: pseudomonas > staph aureus > proteus > fungal (10%) (aspergillus in 80-90%; klebsiella, candida); enterobacter Symptoms: pain, discharge, conductive hearing loss; tenderness on pinna movement Management: combined steroid / antibiotic ear drops for 1/52 (eg. Dexamethasone + framycetin + gramicidin); ciprofloxacin TOP if treatment failure / tympanic membrane perforation / T tubes in situ Give systemic antibiotics if: fever and systemic symptoms, involvement of pinna, folliculitis; flucloxacillin 12.5mg/kg QID PO for 5/7 Debridement / mopping if: significant debris, ear toilet (gentle irrigation with hydrogen peroxide and Suctioning Wick insertion if: mod/severe, replaced Q2days Daily review until improvement Malignant otitis externa: invasive form; pseudomonas in >90%; risk factors = diabetes, immunosuppression; suspect if persistent otitis externa for >2-3/52; may cause otitis media of base of skull, mastoid air cells, sigmoid sinus, parotid gland facial paralysis, cranial nerve VII cranial nerve X, X, XI; lateral / sigmoid sinus thrombosis, meningitis; do CT; give IV gentamicin 5mg/kg OD + ceftazidime 2g TDS or ciprofloxacin 400mg BD, admit