Electronic supplementary material Early blood lactate area as a
advertisement
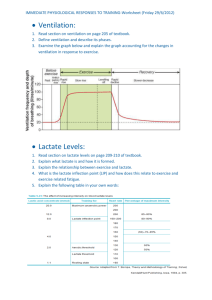
Electronic supplementary material Early blood lactate area as a prognostic marker in pediatric septic shock Young A Kim, Eun-Ju Ha, Won Kyoung Jhang, Seong Jong Park Division of Pediatric Critical Care Medicine, Department of Pediatrics, Asan Medical Center Children’s Hospital, University of Ulsan College of Medicine, Seoul, Republic of Korea Supplement to methods The institutional review board of Asan Medical Center approved the study protocol and waived the requirement for informed consent (20120512). Supplement to results Patients Four patients were excluded according to the exclusion criteria. One patient with primary liver failure of unknown origin and one patient with MELAS were excluded. Two patients whose hospital stay was shorter than 24 hours, were also excluded. Six patients received bone marrow transplantation and two of these patients died. Four patients had undergone liver transplantation at least one year previously due to Budd-Chiari syndrome (n = 1), biliary atresia (n = 2) or fulminant hepatitis (n = 1) and they were all on immunosuppressive agents. Relationship between clinical variables The relationship of the lactate variables with the PRISM III score, PELOD score and the number of organ dysfunctions were determined by calculating the Spearman correlation coefficient and the twotailed significance. There was a significant correlation between the PRISM III score and the lactate variables (vs. initial lactate: r = 0.521, p < 0.001; vs. lactate clearance: r = -0.582, p < 0.001; vs. lactate area: r = 0.702, p < 0.001). There was also a significant correlation of the PELOD score, the initial lactate level, and the lactate area (vs. initial lactate: r = 0.435, p < 0.001; vs. lactate clearance: r = -0.141, p = 0.270; vs. lactate area: r = 0.503, p < 0.001). The number of organ dysfunctions and lactate variables also showed a significant correlation (vs. initial lactate: r = 0.261, p = 0.036; vs. lactate clearance: r = 0.394, p = 0.01; vs. lactate area: r = 0.472, p < 0.001). Supplement to discussion The overall mortality rate of our study patients was higher than that seen in previous studies of pediatric severe sepsis [1, 2]. As our medical center is a tertiary referral center, most of our patients have underlying co-morbidities with a high proportion of hemato-oncologic disease and a high severity of illness. In this study, most of the patients were admitted to the PICU in an advanced state of disease and with multiple organ dysfunction with a higher mean PRISM III score, and thus requiring more ventilatory support and inotropic/vasoactive agents, compared with the patients seen in a previous study [2]. Referances 1. Watson RS, Carcillo JA, Linde-Zwirble WT, Clermont G, Lidicker J, Angus DC (2003) The epidemiology of severe sepsis in children in the United States. Am J Respir Crit Care Med 167:695-701 2. Kutko MC, Calarco MP, Flaherty MB, Helmrich RF, Ushay HM, Pon S, Greenwald BM (2003) Mortality rates in pediatric septic shock with and without multiple organ system failure. Pediatr Crit Care Med 4:333-337 Table E1. The area under the curve of the lactate levels at each time point as a predictor of mortality. Variables AUC P value 95% CI 6-hr lactate 0.790 < 0.001 0.659 – 0.921 12-hr lactate 0.852 < 0.001 0.743 – 0.960 18-hr lactate 0.866 < 0.001 0.760 – 0.973 24-hr lactate 0.831 < 0.001 0.719 – 0.942 Figure E1. The KaplanMeier survival curves for the lactate area of the patient groups as measured above and below 96 mmol/lh. Their survival was followed for 28 days. The log rank test was performed (p = 0.004).