Lactate Acidosis
advertisement

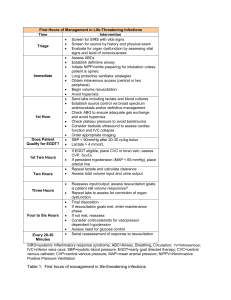
Lactate Acidosis 9/5/10 PY OH - hyperlactaemia: a level from 2 to 5 mmol/L - severe lactic acidosis: > 5 mmol/L (mortality very high) - high mortality with lactate > 8mmol/L PHYSIOLOGY Daily production - normal production = 20 mmols/kg/day) -> blood -> hepatic and renal metabolism (Cori cycle) - all tissues can produce lactate under anaerobic conditions. Relationship of lactate to pyruvate Pyruvate + NADH + H+ <=> Lactate + NAD+ - catalysed by lactate dehydrogenase - pyruvate and lactate are in equilibrium - lactic acid has a pK value of about 4 so it is fully dissociated into lactate and H+ at body pH Tissues Producing Excess Lactate - at rest, the tissues which normally produce excess lactate are: (i) skin - 25% of production (ii) red cells - 20% (iii) brain - 20% (iv) muscle - 25% (v) gut - 10% - during heavy exercise, the skeletal muscles contribute most of the much increased circulating lactate. - during pregnancy, the placenta is an important producer of lactate (can pass to fetus as well). Lactate metabolism and elimination - lactate is metabolised predominantly in the liver (60%) and kidney (30%). 50% -> glucose (gluconeogenesis) and 50% -> CO2 and water (citric acid cycle) this results in no net acid accumulation but requires the aerobic metabolism the small amount of lactate that is filtered (180mmol/day) is fully reabsorbed. Jeremy Fernando (2010) PATHOPHYSIOLOGY - lactic acidosis can occur due to: (i) excessive tissue lactate production (ii) impaired hepatic metabolism of lactate (large capacity to clear) - clinically there is often a combination of the above to produce a persistent lactic acidosis CAUSES (Cohen & Woods classification) Type A - Inadequate Oxygen Delivery (i) anaerobic muscular activity (sprinting, generalised convulsions) (ii) tissue hypoperfusion (shock, cardiac arrest, regional hypoperfusion -> mesenteric ischaemia) (iii) reduced tissue oxygen delivery (hypoxaemia, anaemia) or utilisation (CO poisoning) Type B - No Evidence of Inadequate Tissue Oxygen Delivery B1: associated with underlying diseases - LUKE: leukaemia, lymphoma - TIPS: thiamine deficiency, infection, pancreatitis, short bowel syndrome - FAILURES: hepatic, renal, diabetic failures B2: associated with drugs & toxins - phenformin cyanide beta-agonists methanol adrenaline salicylates nitroprusside infusion ethanol intoxication in chronic alcoholics anti-retroviral drugs paracetamol salbutamol biguanides fructose sorbitol xylitol isoniazid B3: associated with inborn errors of metabolism - congenital forms of lactic acidosis with various enzyme defects (eg pyruvate dehydrogenase deficiency) Jeremy Fernando (2010) DIAGNOSIS - plasma lactate level - once documented the cause must be found and treated appropriately - D lactate = isomer of lactate produced by intestinal bacterial and not by humans -> a bed side test may be able to be developed to help with diagnosis of mesenteric ischaemia. MANAGEMENT (i) diagnose and correct the underlying condition (ii) restore adequate tissue oxygen delivery (iii) ensure appropriate compensatory hyperventilation where possible Use of bicarbonate - two randomised controlled studies of bicarbonate in lactic acidosis and shock found no beneficial effects on cardiac function or any other effects of pH correction. - types available: NaHCO3, carbicarb, dichloroacetate, Tris/THAM - only real justification in the treatment of acidosis: severe pulmonary hypertension and right heart failure to optimized right ventricular function and severe IHD where lactic acidosis is thought to be an arrythmogenic risk. Adverse effects: - acute hypercapnia - ionised hypocalcaemia - intracellular acidosis due to CO2 crossing cell membranes rapidly - acute intravascular overload - bicarbonate increases lactate production by increasing the activity of the rate limiting enzyme phosphofructokinase, shifts Hb-O2 dissociation curve, increased oxygen affinity of haemoglobin and thereby decreases oxygen delivery to tissues Indications: (i) patients with pulmonary hypertension in whom pulmonary vasoconstriction may be worsened by acidosis (ii) patients with significant ischaemic heart disease in whom severe acidosis lowers the threshold for arrhythmia Dialysis/haemofiltration - peritoneal dialysis is not useful in removing lactate when using bicarbonate buffered - haemofiltration: it remains a useful marker of clinical disease progression in patients on bicarbonate buffered haemofiltration Jeremy Fernando (2010)