Septic shock
Septic Shock
SCOPE (Area):Emergency Department
SCOPE (Staff): Emergency Staff
PURPOSE and SCOPE : To educate staff and ensure patients with severe sepsis and septic shock are identified and aggressively managed.
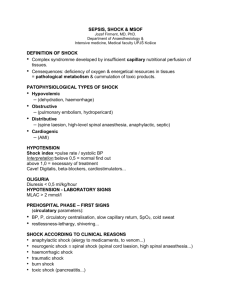
DEFINITIONS
Sepsis : Infection, documented or suspected and some of the following;
General
Fever (>38.3), hypothermia (<36), Tachycardia > 90
Tachypnoea, altered mental status, significant oedema
Hyperglycaemia in absence of Diabetes mellitus
Inflammatory variables
Leukocyctosis/penia (<4, >12), or normal WBC with >10% immature forms
CRP elevated
Haemodynamic variables
SBP < 90, MAP <70 or an SBP decrease >40 in adults (units mmHg).
Organ dysfunction
Arterial hypoxemia (pao2/Fi02<300), acute oliguria, Creatinine increase
Coagulation abnormalities, ileus, thrombocytopenia, elevated bilirubin.
Tissue perfusion variables
Hyperlactatemia, decreased capillary refill.
Severe sepsis : Sepsis-induced tissue hypoperfusion or organ dysfunction (any of the following thought to be due to infection).
Sepsis induced hypotension
Elevated lactate
Low Urine Output
Acute lung injury with Pa02/Pio2 <250 in absence of pneumonia or <200 in presence of pneumonia
Elevated creatinine, bilirubin platelet count, coagulopathy.
PROCEDURE
Treatment priorities:
Resuscitation
Early treatment with antibiotics (first hour) and/or surgical drainage of infection.
Early initiation of supportive care to correct physiologic abnormalities including hypoxemia and hypotension.
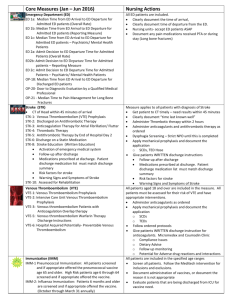
To be completed within 3 hours
Measure lactate
Obtain blood cultures
Administer antibiotics
Administer 30mls/kg crystalloid for hypotension or lactate >4
Referral to ICU/inpatient unit/consideration of surgical intervention
To be completed within 6 hours
Apply vasopressors – for hypotension not responding to fluids; MAP>/ 65mmHg
In the event of persistent hypotension despite volume resus or initial lactate >/ 4 o Measure CVP – aim > 8mmHg
Remeasure lactate if initial lactate level was elevated.
CPG/I2.12.03: Septic Shock (2017
) Page 1 of 2
Management:
1.
Resuscitation – for hypotension or hypoperfusion (lactate >4) o Fluid therapy – resuscitation with IV crystalloid (normal saline) for sepsis induced hypoperfusion with suspicion of hypovolemia to achieve a minimum of 30mls per kg of fluid. Reassess after each 250 - 500mls for response – escalate treatment with each failure to respond. IVF are a preference as long as they increase perfusion without seriously impairing gas exchange. o Following initial fluid resuscitation reassessment of ABC is required. Ongoing signs of septic shock require invasive monitoring – arterial line, central venous pressure monitoring and urinary catheter – in addition to standard monitoring. o Vasopressor – noradrenaline centrally administered is the vasopressor of choice. Use adrenaline as the first aline agent in septic shock when blood pressure is poorly responsive to NA. o End points (resuscitation goals within 6 hrs)
MAP > 65mmHg.
CVP of 8-12mmHg (If MAP < 65mmHg)
UO > 0.5mls/kg/hr
2.
Antimicrobial therapy - within the first HOUR of recognition of severe sepsis. o Basic investigations and cultures – standard bloods, blood cultures – 3 sets are optimal, CXR, urine culture, sputum, swabs – vaginal, oral, lumbar puncture. o Treatment – administer antibiotics early . Empiric broad spectrum antibiotics
(as per antibiotic guidelines) when a definite source is not identified. o Surgical involvement early for necrotising infections, abscesses or other appropriate conditions.
3.
Other management to consider o Source control – e.g. necrotizing soft tissue infections, cholangitis, emphysema
– be sought and diagnosed and intervention undertaken. o Mechanical ventilation – target TV of 6mls/kg, permissive hypercapnoea to minimise plateau pressures and TV, apply PEEP, elevate head of bed. o PPE and isolation rooms should be considered where the likely pathogen poses an infectious risk to staff or other patients, this includes use of N95 masks for staff when intubating patients, inline suctioning and filters o Supportive care – general management of the likely immobilized critical care patient –glucose control, DVT prophylaxis, nutrition, pressure care. o Corticosteroids – for adrenal insufficiency, or patients already on steroid therapy o Blood products for HB < 70 o Identification of special groups – e.g. immunocompromised, neutropenic, tropical infections (refugee groups, returned traveller), pregnant patients.
Disposition – intensive care environment.
Consultation with appropriate units – e.g. infectious diseases, surgical unit.
REFERENCES
Alan E Jones, MD; Michael A Puskarich, MD. The Surviving Sepsis Campaign Guidelines 2012: Update for
Emergency Physicians. Annals of Emergency Medicine. 2013 1-13.
Reg. Authority: Director & NUM Emergency Medicine
Review Responsibility: Emergency Department
Original Author: unknown 2004
Updated by: Dr E West 2010,2014
Date Effective: 14.2.2014
Date for Review: 2.2017
CPG/I2.12.03: Septic Shock (2017
) Page 2 of 2