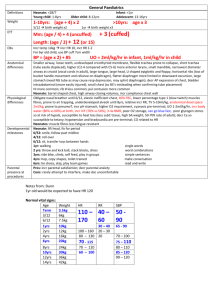
Lithium overdose fact sheet
advertisement

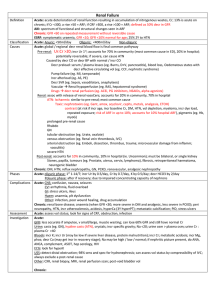
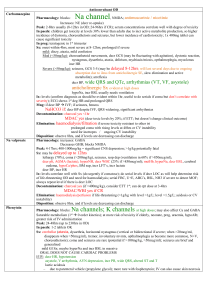
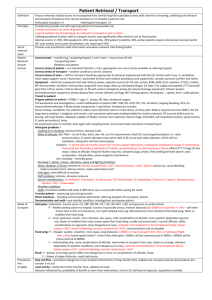
LITHIUM OVERDOSE Charcoal ineffective Pathophysiology Therapeutic dose: 300 – 2700mg/day Therapeutic levels: 0.6-1.2mmol/L; peak in 2-4hrs (6-8hrs if SR) Acute toxic dose: if normal renal function and Na, acute OD usually tolerated quite well; toxicity determined by rate of rise of serum levels >2500mg (>40mg/kg) GI Sx, but rarely neuro Sx Chronic toxic dose: more severe Sx at lower levels >1.5mmol/L = toxicity Drug properties: Low therapeutic index; renal clearance (small deterioration in renal function large effect on Li elimination); elimination half life 1227hrs; suitable for dialysis (small molecular size, high water solubility, lack of metabolites, little protein binding) Causes: usually due to decr GFR (eg. thiazides, NSAIDs, ACEi, SSRI, sepsis, hypotension, dehydration, CCF); hypoNa ( incr Li reabsorption) Drug interactions: haloperidol + phenothiazides ( NMS like effect), methyldopa ( Parkinsonian), NM blockers ( prolonged DOA) Effects of chronic use: alters urinary concentrating ability nephrogenic DI; competes with Na + K for reabsorption; blunts response of thirst centre to dehydration; causes hypothyroidism Toxicity Acute: mimics gastro / flu; Sx may have 3-5/7 delay in onset GI Sx more common (N+D+AP, polydipsia, polyuria) significant fluid loss; GI Sx correlate well with levels (unlike in Fe) CV Sx (HB, prolonged QTc; usually not assoc with significant CV effects) Neuro Sx uncommon (but more likely if severe / delayed presentation / renal failure / dehydrated) Chronic: occurs following change in dose Neurotoxicity more common; may be permanent GI Sx uncommon Assessment Mng = N+V, fine intention tremor (most common and earliest); lethargy, memory and conc probs Grade 1 (mild): <1.5mmol/L Grade 2 (mod): 1.5-2.5mmol/L = hyperreflexia / hypertonia, coarse resting tremor, ataxia / dysarthria, weakness, visual probs, agitation / confusion, fasciculations 2.5-3.5mmol/L = rigidity / myoclonus, incr / decr tone, choreoathetosis, nystagmus, stupor, decr BP Grade 3 Isevere): >3.5mmol/L = seizures, flaccid paralysis, coma, ARF Consider in any patient on lithium who presents unwell / with neuro Sx; look for precipitating illness Differential diagnosis: non-convulsive status, SS, NMS, electrolyte abnormality, CNS pathology Investigations: Li level (less helpful in acute poisoning, used to make diagnosis only; guide to trt in chronic), U+E (decr K, low AG, decr/incr Na, acidosis), FBC (chronic Li use neutrophilia, WBC 10-15); ECG (chronic Li use T wave flattening and inversion; toxicity long PR, QRS, QTc); AXR Indications for GI decontamination: acute overdose + >40mg/kg ingested / tablets on AXR + within 1-2hrs ingestion Use PEG; resonium may incr rate of Li elimination >6mmol/L (acute) / >2.5mmol/L (chronic) Indications for dialysis: Li level Severe clinical Sx (esp neuro Sx: coma / seizures) with high level ARF even if lower level Decr BP not responding to fluids Mostly used in chronic / delayed presentation acute; will need to be prolonged as slow equilibration time between intraC and extraC; may get rebound incr level on stopping; serial Li levels helpful; no evidence that haemodialysis improves outcome May increase effect of sux and vec Prognosis Other trt: in acute – give IVF (aim UO >1ml/kg/hr) to help Li diuresis, decr intracellular Li levels; stop interacting drugs Disposition: discharge if: acute ingestion + asymptomatic + peak level <1.5mmol/L Prolonged observation if: SR If treated, discharge once: level <2 Good prognosis: GI Sx only Notes from: Dunn, Cameron, Tox Book