Immunohistochemical staining of the brain tissue
advertisement

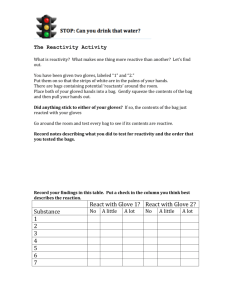
Ref - Furukawa S, Morita S, Wingenfeld L, Matsuda W, Nakagawa T, Sakaguchi I, Takaya A, Nishi K. Immunohistochemical staining of the brain tissue obtained from a man with multiple focal brain infarctions and different staging. Anil Aggrawal's Internet Journal of Forensic Medicine and Toxicology [serial online], 2014; Vol. 15, No. 1 (Jan - June 2014): [about 16 p]. Available from: http://anilaggrawal.com/ij/vol_015_no_001/papers/paper002.ht ml. Access the journal at - http://anilaggrawal.com ********************************************************************* Title Immunohistochemical staining of the brain tissue obtained from a man with multiple focal brain infarctions and different staging Satoshi Furukawa, Satomu Morita, *Lisa Wingenfeld, Wakoto Matsuda, Tokiko Nakagawa, Ikuo Sakaguchi, Akari Takaya, Katsuji Nishi Department of Legal Medicine, Shiga University of Medical Science, Shiga Japan *Institute of Legal Medicine, Munich University, Munich, Germany Satoshi Furukawa Department of Legal Medicine, Shiga University of Medical Science, Shiga Japan Setatsukinowa, Otsu, Shiga 520-2192, Japan 31041220@belle.shiga-med.ac.jp TEL/FAX; +81775482200 Abstract We encountered an autopsy case of a 65-year old male with multiple infarct legions in his brain. The stage of infarctions were different, that is, infarction with bleeding, necrotic and cavity, respectively. We examined morphological and immunohistochemical study of each legion using antibodies against CIRP, RBM3, HSP70, HIF1, VEGF, e-NOs, AIF1, p53, c-Fos, CCC9 and SIRT1. The results indicate that CIRP and RBM3 may play an important role of prevention of hypoxic status. The reactivity of RBM3 in the infarct legions was detected in early stage, and increased with progress of the stages of infarcts. And RBM3 may also play an important role in the angiogenesis in the infarct area. SIRT1 was expressed in the neurons or glial cells surrounding of infract legions especially in late stage, showing the expression of SIRT1 was delayed than those of CIRP and RBM3. KeyWords: Multiple brain infarctions, Hypoxia, Immunohistochemical staining, Introduction There were many studies on histological characteristics of brain infarctions (1-4). We also made a study concerning the immunohistochemical staining figures on the chronic brain infarction(5). Although chronic infarctions with tissue defect in the brain were often detected in the forensic autopsy cases from elder victims, detection of the focal infarction with bleeding was rare. We experienced an autopsy case in which a 65-year-old male had multiple focal infarctions with different staging, and we made immnuhistochemical staining of the brain tissues using antibodies to resolve the roles of hypoxia, ischemic and stress related antigens and inflammation materials on the progress of the brain infarction. It is widely accepted that in hypoxia and ischemic cases an increase in the transcription level of specific genes, including those encoding for hypoxia-inducing factor 1(HIF1), apoptotic inducing factors (AIF-1), and stress related factors containing Cold inducing RNA binding protein (CIRBP) and RNA binding motif 3 (RBM3) which are recognized as a cold stress inducing protein and were intensively expressed in the postmortem human heart muscle obtained from accidental hypothermic death cases (1-6). Neuroglobin (Ngb) , Complement component C 9 , c-Fos , Protein 53 (p53) , Sirtuin 1 (SIRT1) and Heat shock protein 70 (HSP70) were also expect to express in the hypoxia or ischemic brain area(7-13). Materials and methods Autopsy case A 65-year-old male was a victim. Although he has been thinking that he remains unmarried for his life after his parent’s death, he had a formal meeting with a view to marriage the last year. The next day of the meeting he married with 45-year-old female who had one sun. After one week of his marriage he was found death in his living room when his wife and sun came back to home after looking their jobs. The police suspected the criminal. The police investigation revealed that there was one visitor who was his relative during their absence and he has been suffering from diabetes, liver, kidney and heart. At autopsy, the chronic infarctions in the right-frontal lobe and right-cerebellum were recognized and subacute one was detected right-basal ganglion, and additionally newly infarction with small amount of bleeding was seen in left-cerebral cortex. Histology Each brain tissue cut at autopsy was fixed in formalin and prepared paraffin blocks within three days after autopsy. Stainability of Macrophage, lymphocytes, neurons and astroglia involved in brain infarction were studied by immunohistochemistry using ABC technique (Nichirei, Japan), and antibodies against CIRP, RBM3, HSP70, HIF1, VEGF, e-NOs, AIF1, cFos, Ngb, Wnt, CCC9, carbindinand SIRT1.Immunohistochemical staining with antibodies was performed, according to the manufacture protocol. The characteristics of the antibodies used were described in Table 1. Results 1: Fresh infarction with abundant bleeding The infarcted area has severe bleeding containing large number of intact erythrocytes and small number of macrophages. Anti CIRBP, RBM3 and HSP70 stained macrophage, but not neutrophills, erythrocytes, and endothelium of blood vessels. The reactivity with these antibodies was detected in the neurons and glias around the infarcted area. The staining intensity by anti RBM3 was intensive among these antibodies. Anti HIF1 showed weak reactivity with the neurons and glias around the bleeding area, anti VEGF and e-NOs showed the similar reactivity with the cells around bleeding area, the staining intensity among these antibodies was remarkable by anti e-NOs, and these antibodies showed no reactivity with vascular endothelial cells. Anti AIF1, Ngb, Wnt, cFos, CCC9, p53 and SIRT1 showed no reactivity in the bleeding area. Anti SIRT 1 showed moderate reactivity with neurons and glias around bleeding. Anti CCC9 showed weak reactivity with these cells. The other antibodies showed a feeble or no reactivity. 2: Semi-chronic infarction Semi-chronic infarction might be subdivided into two phases. 2-1: Phase of acute infarction HE staining showed the presence of coagulative necrosis, spheroids, mononuclear cells, macrophages and gemistocytes, however remarkable neo-angiogenesis and inflammatory cells were not detected in this patient. Anti RBM3 showed clear reactivity with nucleus of vascular endothelial cells and other type of cells, such as macrophages and mononuclear cells. Anti CIRBP and HSP70 showed the similar stainability but were relatively weak(Figure.1). Anti eNOs showed similar reactivity with those by anti RBM3, however anti HIF1 and VEGF showed feeble or very weak reactivity in the lesion (Figure.2). Anti SIRT1 showed weak or a feeble reactivity with nucleus in the cell group containing giant granular corpuscle cells in the infarct area. Anti CCC9 showed intensive reactivity with some cells that were pyramidal shape and not able to identified, and the antibody also showed clear reactivity with the giant granular corpuscle cells in the infarction area. The other antibodies showed feeble or no reactivity in the lesion. 2-2: Phase of subacute infarction HE staining revealed amorphous, granular, pink material、fibrous cells and gemistocytes in which the ghost outlines of some necrotic neurons could be detected in semi-chronic infarction area. Although angiogenesis and abundant of macrophages were observed, perivascular inflammatory mononuclear cells were not remarkable in this patient. Anti RBM3 clearly stained nucleus in the many type of the cells inside the infraction area, and the cells that were adhered to the angiogenesis capillary walls (Figure.3). Anti CIRBP and HSP70 showed the similar stainability with relatively weak. Although anti HIF1 and VEGF showed weak reactivity with the several kinds of cells inside the infarction area, anti e-NOs showed moderate reactivity with these cells (Figure.4). Anti SIRT1 showed clear reactivity with the nucleuses of the cell group containing giant granular corpuscle cells in the infarct area, while the antibody showed weak reactivity the cells outside infarction area. Anti AIF1, cFos and Ngb showed weak reactivity with the cells inside the infarction area, p53 and Wnt showed feeble or no reactivity. Anti CCC9 showed no reactivity in the infarct area and clear reactivity with the giant granular corpuscle cells outside the infarction area (Figure.5). 3: Chronic infarction in the cerebellum (resorption phase) Since this patient had the cerebellum with a large cavitation, the infarct area in the cerebellum was used to investigate. HE staining revealed a cystic space from the resolvedliquefactive necrosis, hemosiderin pigments, compound granular corpuscle cells and macrophages in chronic infarction area. Anti CIRBP, RBM3 and HSP70 showed feeble reactivity with the scattered cells in the liquefactive necrotic area, and anti RBM3 and CIRBP showed weak reactivity with the nucleus of cells in the arterial walls. These antibodies reacted with giant granular corpuscle cells around the necrotic area. Anti HIF1, VEGF and e-NOs showed the cells around infarct area and no in the cavitation. Anti c-Fos, p53, CCC9 and SIRT1 showed a feeble or no reactivity in this area. Discussion The report concerning to immunohistochemical study on multiple brain infarction with several stages are very few. In this case, patient with multiple infarct lesions with bleeding, numerous macrophages, necrosis, neo-vascularization and cavitation in infarction lesions, respectively, presumed to die due to cardiac fibrillation, since the small thrombosis in blood vessel near by fresh infarct with bleeding and in right coronary artery were detected, and then multi-focal infarctions presumed to be originated from his heart. First, we were able to group each lesion into three categories according to Mena et al (14). However in this case, peri-vascular cuffing was not clearly detected, although morphological changes could be agreed to the described findings. In this study, anti RBM3 showed clear and intensive reactivity in the infarct area. RBM3 was also expressed in the nucleuses on the macrophage, and neutrophils and CIRBP and HSP 70 reactivity were also recognized in the glial and/or neural cells detected around the infarct area. These results indicate the expression of RBM3, CIRBP and HSP70 may relate to hypoxia or ischemic situation, although RBM3 and CIRBP were accepted as cold inducible antigens and these were expressed in the cardiac muscle obtained from individuals who died due to accidental hypothermia (11). It is well accepted that HIF1 which closely relate with hypoxia controls or manages to expression of VEGF, and the expression of VEGF is connected with the expression of e-NOs, since Qing et al have proposed that the response to hypoxia is primarily mediated by the transcription factor hypoxia-inducible factor-1 (HIF-1) which leads to the induction of a variety of adaptive gene products including vascular endothelial growth factor (VEGF) and endothelial nitric oxide synthase (eNOS) (15). In this study the expression of RBM3 was detected in the endothelial cells of the blood vessels in the acute or subacute infarct area, showing similar to those in VEGF and e-NOs. These results indicate that RBM3 may also play an important role in the angiogenesis in the infarct brain area. Several studies have implicated the protection effect of SIRT1 against ischemic insult in the heart. We also showed that SIRT1 expressed in the hearts obtained from individuals who died due to hypothermic and carbon monoxide poisoning. Although expression of SIRT1 in the brain was not or weakly detected in our previous studies which were performed using the brains obtained from victims who died due to self-strangulation, hanging and/or manual strangulation, the existence in the nucleuses in the cells of around infract area was clearly recognized in this case. The prolonging of hypoxic and/or ischemic situation occurred in his brain may bring out the increasing of transcription of SIRT1. SIRT1 may also play an important in neuroprotection. References 1). Palm DE, Knuckey NW, Primiano MJ, Spangenberger AG, Johason CE. Cystatin C, a protease inhibitor, in degenerating rat hippocampal neurons following transient forebrain ischemia.BrainRes.1995; 691: 1-8. 2). Yamashima T. Implication of cysteine proteases calpain, cathepsin and caspase in ischemic neuronal death of primates. ProgNeurobiol. 2000; 62:273-95 3). PalmDE.,Knuckey NW., Primiano MJ., Spangenberger AG., Johanson CE., Cystatin C, a protease inhibitor, in degenerating rat hippocampal neurons of following transient forebrain ischemia. Brain Res, 1995; 691: 1-8. 4). Sairanen T., Ristimaki A., Karjalainen-Lindsberg ML., Paetau A., Kaste M., Lindsberu PJ. Cyclooxygenase-2 is induced globally in infarcted human brain. Ann Neurol. 1998; 43: 738-47. 5). Kobayashi A.K, Talase I, Kitamura T, Takamure A, Nakagawa T, Ohyagi M, Morimoto A, Yamasaki S, Yamomoto Y, Ohkubo I, Nishi k. Immunohistochemical characteristics of necrotic area in the old-infarction area of humanbrain by using antibodies against cystatin C, Cathepsin B, puromycine sensitive alanyl-aminopeptidase and prostaglandin D2 synthase. Anil Aggrawal's Internet Journal of Forensic Medicine and Toxicology, 2007; Vol. 8, No. 1 (January - June 2007): http://www.anilaggrawal.com/ij/vol_008_no_001/papers/p aper001.html 6). Wang G L, Rue E A, Semenza G L, Hypoxia- inducible factor 1 is a basic-helix-loop-helix-PAS hereodimer regulated by cellular O2 tension. Pro NatlAcdSci USA, 1995; 92: 5510-5514. 7). Smith T G, Robbins PA, Ratclife PJ, The human side of hypoxia-inducible factor, Br,J.Haematol, 2008; 141: 325-334. 8). Joza N, Susin SA, Daugas E, Stanford W L, Cho S K, Li C Y, Sasaki T, Elia A J, Cheng H Y, Ravagnan L, Ferri K F, Zamzami N, Wakeham A, Hakem R, Yoshida H, Kong Y Y, Mak T W, Zuniga-Pfluecker J C, Kromer G, Penninger J M, Essential role of the mitochondrial apoptosis-inducing factor in programmed cell death. Nature 2001; 6828: 549-554. 9). Nishiyama H, Higashitsuji H, Yokoi H, Itoh K, Danno S, Matsuda T, Fujita J, Cloning and characterization of human CIRBP. cold-inducible RNA-binding protein cDNA and chromosomal assignment of the gene. Gene, 1998; 204: 115-120. 10). Derry J M, Kerns J A, Francke U, RBM3, a novel human gene in Xp11.23 with a putative RNA-binding domain, Hum Mol Genet 1996; 4: 2307-2311. 11). Furukawa S, Wingenfeld L, Sakaguchi I, Nakagawa T, Takaya A, Morita S, Yamasaki S, Nishi K, Histopathological characteristics of human cardiac tissues in accidental hypothermia using immunohistochemistry; Immunohistochemical detections of cold, hypoxia and apoptotic related antigens are practicable in the myocardium from hypothermic death even in postmortem examination, Anil Aggrawal's Internet Journal of Forensic Medicine and Toxicology, 2013; Vol. 14, No. 1 :http://www.anilaggrawal.com/ij/vol_014_no_001/main.ht ml 12). Burmester T, Hankeln T, What is the function of neuroglobin, J ExpBiol, 2009; 212: 1423-1428. 13). Fracasso T, Pfeiffer H, Michaud K, Koehler H, Sauerland C, Schmeling A, Immunohistochemical expression of fibronectin and C5b-p in the myocardium in cases of carbon monoxide poisoning. Int J Legal Med, 2011; 125: 377-384. 14). Mena H, Cadavid D, Rushing E L, Human cerebral infarct: a proposed histopathologic classification based on 137cases, ActaNeuropathol, 2004; 108: 524-530. 15). Qing M, Goeriach M, Schumacher K, Woeltje M, Vazquez-Jimenez J F, Hess J, Seghaye M C, The hypoxia-inducible factor HIF-1 promotes intramyocardial expression of VEGF in infants with congenital cardiac defects. Baisc Res Cardiol, 2007; 102: 224-232.