Perianal Problems
advertisement

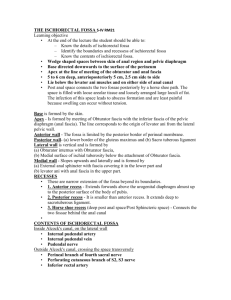
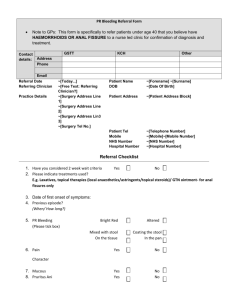
Perianal Problems Haemorrhoids Definition: prolapse of mucosa of anal canal, associated with congestion of superior haemorrhoidal venous plexus; due to straining and high sphincter tone Positions: R anterior, R posterior, L lateral perianal > ischiorectal > intersphincteric, submucosal, high intermuscular > supralevator Degrees: 1st degree (bleed, but no prolapse); 2nd degree (prolapse on straining); 3rd degree (persistently prolapsed); 4th degree (irreducible); internal occur proximal to dentate line Complications: haemorrhage, thrombosis, perianal irritation Investigations: indications for colonoscopy: Fe deficiency anaemia, +ive FOB, >40yrs with FH bowel cancer, >50yrs with no recent colonscopy Management: reduce prolapse, warm baths, topical analgesia / steroid, stool softeners; injection for 1 st and 2nd degree haemorrhage control (complications – pain, ulceration, intra-mucosal injection, haemorrhage from sup haemorrhoidal artery, abscess); thrombosed external haemorrhoids can be excised under LA Indications for OT: 3rd degree; 2nd degree when prolapse is major problem or failed sclerotherapy; strangulation Anal Fissure Definition: triangular tear at anal verge after passage of constipated stools; often point away from anal verge; originate in skin and rarely extend to valves Position: posterior (90% males, 60% females) Acute: painful, superficial Chronic: deep Symptoms: pain on defecation, small amounts of bright red bleeding, constipation Management: LA ointment; GTN ointment has been used with some success; sphincterotomy or anal stretch for chronic Perianal Haematoma (external haemorrhoid) Definition: acute rupture of tributary of inferior haemorrhoidal plexus under perianal skin Symptoms: pain after straining, lump; may rupture / ulcerate Management: analgesia, ice, LA; usually resolve within 1//52; may need cruciate incision and drainage Perianal Abscess Anal Fistula Pilonidal Abscess Cause: Staph, E coli, Proteus; from anal fissure, perianal haematoma, haemorrhoid injection site, hair follice, anal gland Risk Factors: ulcerative colitis, Crohn’s disease, diabetes, cancer Types: perianal (most common; superficial to anal margin); ischiorectal (between anus and sphincters medially, and obturator internus laterally); submucous / intersphincteric; pelvirectal / supralevator (above levator ani, below pelvic peritoneum) Symptoms: pain, fever, discharge Management: incision and drainage under GA; may need antibiotics if rheumatic heart disease, diabetes, immunocompromised, prosthetic device Definition: abnormal connection between anus and skin; occurs in 50% abscesses Symptoms: discharge, itch, recurrent abscesses Management: incision and drainage Definition: localised infection in natal cleft; usually due to ingrowing hairs Symptoms: pain, fever, local infection Management: analgesia, antibiotics, excision