Anorectal disease
advertisement
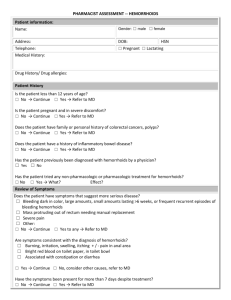
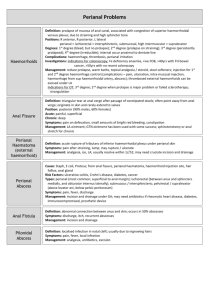
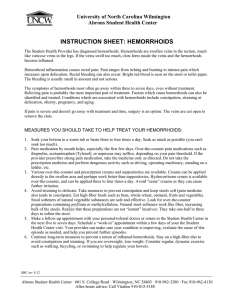
Ahmad kachooei Assistant Professor of Qom Medical University Any patient with anal/perianal symptoms requires a careful history and physical, including a digital rectal examination defecography, manometry, CT scan, MRI, contrast enema, endoscopy, endoanal ultrasound, or examination under anesthesia may be required to arrive at an accurate diagnosis Hemorrhoids are cushions of submucosal tissue containing venules, arterioles, and smooth-muscle fibers . Three hemorrhoidal cushions : 1. left lateral 2. right anterior 3. right posterior continence mechanism aid in complete closure of the anal canal at rest Because hemorrhoids are a normal part of anorectal anatomy, treatment is only indicated if they become symptomatic. Excessive straining increased abdominal pressure hard stools External hemorrhoids are located distal to the dentate line and are covered with anoderm Internal hemorrhoids are located proximal to the dentate line and covered by insensate anorectal mucosa Graded according to the extent of prolapse: First-degree hemorrhoids bulge into the anal canal and may prolapse beyond the dentate line on straining. Second-degree hemorrhoids prolapse through the anus but reduce spontaneously Third-degree hemorrhoids prolapse through the anal canal and require manual reduction. Fourth-degree hemorrhoids prolapse but cannot be reduced and are at risk for strangulation Combined internal and external hemorrhoids straddle the dentate line and have characteristics of both internal and external hemorrhoids Hemorrhoidectomy often is required for large, symptomatic, combined hemorrhoids. result from straining during labor, which results in edema, thrombosis, and/or strangulation. Hemorrhoidectomy is often the treatment of choice, especially if the patient has had chronic hemorrhoidal symptoms Medical Therapy: Bleeding from first- and second-degree hemorrhoids often improves with the addition of dietary fiber, stool softeners, increased fluid intake, and avoidance of straining Associated pruritus may often improve with improved hygiene Rubber Band Ligation Infrared Photocoagulation Sclerotherapy Excision of Thrombosed External Hemorrhoids Closed Submucosal Hemorrhoidectomy Open Hemorrhoidectomy Whitehead's Hemorrhoidectomy Procedure for Prolapse and Hemorrhoids/Stapled Hemorrhoidectomy(PPH) Postoperative pain Urinary retention fecal impaction Bleeding Infection Incontinence anal stenosis ectropion (Whitehead's deformity) A fissure in ano is a tear in the anoderm distal to the dentate line. The vast majority of anal fissures occur in the posterior midline. Ten to 15% occur in the anterior midline. Less than 1% of fissures occur off midline trauma from either the passage of hard stool or prolonged diarrhea. This cycle of pain, spasm, and ischemia contributes to development of a poorly healing wound that becomes a chronic fissure. extremely common tearing pain with defecation and hematochezia (usually described as blood on the toilet paper) painful anal spasm lasting for several hours after a bowel movement can be seen in the anoderm by gently separating the buttocks Patients are often too tender to tolerate digital rectal examination An acute fissure is a superficial tear of the distal anoderm and almost always heals with medical management Chronic fissures develop ulceration and heaped-up edges with the white fibers of the internal anal sphincter visible at the base of the ulcer. There often is an associated external skin tag and/or a hypertrophied anal papilla internally. A lateral location of a chronic anal fissure may be evidence of an underlying disease such as Crohn's disease, HIV, syphilis, tuberculosis, or leukemia. If the diagnosis is in doubt or there is suspicion of another cause for the perianal pain, such as abscess or fistula, an examination under anesthesia may be necessary Therapy focuses on breaking the cycle of pain, spasm, and ischemia First-line therapy to minimize anal trauma includes bulk agents, stool softeners, and warm sitz baths The addition of 2% lidocaine jelly or other analgesic creams can provide additional symptomatic relief. Nitroglycerin ointment (0.2%) Both oral and topical calcium channel blockers (diltiazem and nifedipine) arginine (a nitric oxide donor) topical bethanechol (a muscarinic agonist) Medical therapy is effective in most acute fissures, but will heal only approximately 50 to 60% of chronic fissures. Botulinum toxin (Botox) Surgical therapy: traditionally has been recommended for chronic fissures that have failed medical therapy Approximately 30% of the internal sphincter fibers are divided laterally Healing is achieved in more than 95% of patients by using this technique The majority of anorectal suppurative disease results from infections of the anal glands (cryptoglandular infection) Their ducts traverse the internal sphincter and empty into the anal crypts at the level of the dentate line perianal space 2. intersphincteric space 3. ischiorectal space (ischiorectal fossa) 4. supralevator spaces 1. perianal abscess 2. ischiorectal abscess 3. Intersphincteric abscesses 4. supralevator abscesses 1. Severe anal pain Walking, coughing, or straining can aggravate the pain Palpable mass fever urinary retention life-threatening sepsis Drainage as soon as the diagnosis is established diagnosis is in question:an examination under anesthesia Antibiotics : 1. extensive overlying cellulitis 2. Immunocompromised 3. diabetes mellitus 4. valvular heart disease Drainage of an anorectal abscess results in cure for about 50% of patients. The fistula usually originates in the infected crypt (internal opening) and tracks to the external opening, usually the site of prior drainage. Patients present with persistent drainage from the internal and/or external openings. An indurated tract often is palpable Goodsall's rule can be used as a guide in determining the location of the internal opening . tracks through the distal internal sphincter and intersphincteric space to an external opening near the anal verge often results from an ischiorectal abscess and extends through both the internal and external sphincters originates in the intersphincteric plane and tracks up and around the entire external sphincter originates in the rectal wall and tracks around both sphincters to exit laterally, usually in the ischiorectal fossa The goal of treatment of fistula in ano is eradication of sepsis without sacrificing continence. Simple intersphincteric fistulas often can be treated by fistulotomy (opening the fistulous tract), curettage, and healing by secondary intention seton : Cutting setons 2. noncutting seton endorectal advancement flap :Higher fistulas Fibrin glue 1.