File
advertisement

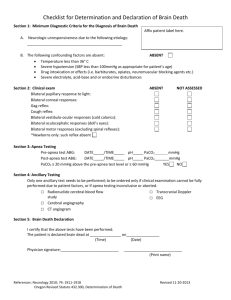
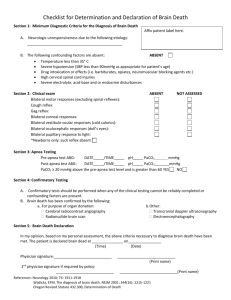
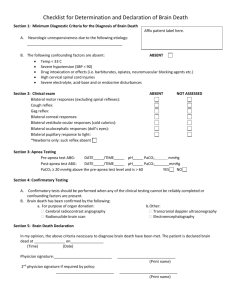
University of Colorado Hospital Policy and Procedure Determination of Death by Neurologic Criteria (Brain Death) Related Policies and Procedures: Organ and Tissue Donation Donation after Cardiac Death Approved by: Description: Patient Care & Assessment Subcommittee Effective: 10/96 Revised: 8/10 This policy states the procedure for determining brain death. Accountability: Brain death is determined by an Attending Neurosurgeon, Neurologist, or Neuro-Intensivist. The determination of brain death must be made in accordance with accepted medical standards and with Colorado Revised Statutes, § 12-36-136. Definitions: A. Brain death: The complete and irreversible cessation of all functions of the entire brain including the brainstem. B. Brainstem reflexes: cranial nerve function is an indicator of brainstem function; reflexes assessed are: pupillary reaction to light, corneal reflex, cough reflex, gag reflex, oculocephalic reflex, oculovestibular reflex, and respiratory reflex. C. Spinal Reflexes: Movements when a sensory stimulus arises from receptors in the muscle, joints, and skin, resulting in a motor response that is entirely contained within the spinal cord D. Coma: state of unarousable, unresponsiveness. Sleep-wake cycles are absent and respiratory patterns are variable and often abnormal. Policies and Procedures: Assure that all reasonable efforts have been made to notify the patient’s healthcare decision maker and family that an examination to determine death will be completed. Arrangements should be made to include the patient’s healthcare decision maker and family in the processes used to determine neurologic death. Involvement of the patient’s healthcare decision maker and family should occur PRIOR to initiation of neurologic death examinations. Legal documentation of death is the time at which death by neurologic exam (brain death) is declared by the Attending neurosurgeon/neurologist/neuro-intensivist. Once death by neurologic criteria has been declared, and the patient is not a potential organ donor, medical means to support the body will be withdrawn. A. Assure the absence of reversible causes of coma. 1. Hypothermia (Core temperature greater than 360 Celsius). 2. No drug intoxication, neuromuscular blockade or poisoning. 3. Exclude metabolic or endocrine disturbances. 4. Radiological evidence of non-survivable brain injury must be documented c150910 Page 1 of 6 Determination of Death by Neurologic Criteria (Brain Death) B. Criteria for determining brain death: (See Brain Death Determination form on page 4. This form is optional for use in declaring brain death. If this form is utilized, it may be placed in the patients chart as documentation. ) Note: The examining physician is not required to perform each and every aspect of the neurological examination in either the American Medical Association or the American Academy of Neurology guidelines, and it is expected that clinical judgment will play a role in each individual case. 1. Unresponsiveness 2. Cerebrally modulated motor responses are absent. Motor responses should be absent after application of painful stimuli. Spinal cord reflexes may be present. Seizures or decorticate/decerebrate posturing rule out a diagnosis of brain death. 3. Absence of the following brainstem reflexes: a. Pupillary reflexes are unresponsive to light b. Corneal Reflexes c. Cough reflex in response to pharyngeal and deep endotracheal suctioning d. Oculovestibular Reflex (Caloric Ice Water Test) e. Respiratory reflex (see apnea testing below) C. Procedure for administering an Apnea Test An apnea test is necessary to support the diagnosis of brain death. The procedure is done by the critical care RN and RT with a physician present during the actual observation period. 1. Prior to Apnea Testing: a. The patient must meet the prerequisites and exam criteria for brain death. b. Have a systolic blood pressure greater than or equal to 100 mmHg. Adjust vasopressors accordingly. c. Obtain baseline ABG d. Oxygen at 100% by mechanical ventilation for at least 10 minutes prior to Apnea Test. Target PaO2 to greater than or equal to 200mmHg e. The ventilator settings should be adjusted for a PaCO2 of 35-45 mmHG f. 2. The Apnea Test begins when mechanical ventilation is removed. Oxygen at 100% should be delivered via t-piece. 3. Monitor blood pressure and heart rate continuously. The test should be terminated if: a. More than 50% increase of current vasopressor dose is required to maintain systolic blood pressor greater than or equal to 90 mmHg b. Symptomatic cardiac arrhythmias develop c. Oxygen saturation measured by pulse oximetry drops below 85% for greater than 30 seconds d. Mechanical ventilation resumed, and an ABG obtained if desired results are not achieved, and alternative confirmatory tests are recommended. . 4. Observe and/or feel for any respiratory effort for 8-10 minutes. If respiratory effort is noted, stop the test and resume mechanical ventilation. The patient does not meet brain death criteria. 5. During the test, the PaCO2 is expected to rise about 3 mmHg/minute during apnea test. The amount of time off the ventilator will depend on the starting PaCO2 level.(is this correct?) The expected PaCO2 endpoint is 60 mmHg or greater OR 20mmHg above baseline. c150910 Page 2 of 6 Determination of Death by Neurologic Criteria (Brain Death) 6. To confirm a brain death diagnosis, an ABG should be drawn at the end of the apnea test to assure the PaCO2 level is within diagnostic range. RESUME VENTILATION. 7. If there is no evidence of respiratory effort AND the PaCO2 is 60mmHg or greater OR 20 mmHg above a known baseline, THEN the apnea test supports the diagnosis of brain death. 8. If the test is inconclusive but the patient is hemodynamically stable during and after the procedure, it may be repeated for a longer period of time (10-15 minutes) after patient has been pre-oxygenated at 100% FiO2 for at least 10 minutes. D. Procedure for administering Cold Caloric test The oculovestibular reflex (cold caloric) is to determine brainstem function of an unconscious patient. The procedure is done by a physician. 1. Each ear canal is irrigated with approximately 50 mL of ice water;observe patient for 1 minute after injection for eye movement and at least 5 minutes between testing on each side. 2. No eye movement indicates brainstem damage. E. Confirmatory tests These tests are not required. These are optional and may be used in conjunction with a clinical exam to support the diagnosis of brain death. They are recommended in any case where the etiology of coma is unclear or the patient is too hemodynamically unstable to perform apnea test. 1. Cerebral Arteriography 2. Radionuclide Scanning 3. Electroencephalogram (EEG) 4. Transcranial Doppler Ultrasonography (TCD) Additional Supportive Information Intracranial Pressure Monitoring: A diagnosis of brain death is supported when patient’s intracranial pressure (ICP) is equal to or greater than the patient’s mean arterial pressure (MAP). Documentation by the Physician 1. Etiology and irreversibility of condition 2. Clinical observations including prerequisite criteria and apnea testing 3. Date and time of death 4. Confirmatory testing methodology and results F. Special considerations: Pediatric patients are required to be evaluated by a pediatric neurologist or neurosurgeon. c150910 Page 3 of 6 Determination of Death by Neurologic Criteria (Brain Death) I am wanting to use this worksheet rather than the original below. It is more detailed and follows a better step by step appraoach University of Colorado Hospital BRAIN DEATH DETERMINATION DOCUMENTATION Have all reasonable efforts been made to notify patient's family or decision maker that a brain death test will be completed? Yes Checklist for determination of brain death 1. Prerequisites (all must be checked) a. Coma, irreversible, and cause known b. Neuroimaging explains coma (if stable to obtain) c. CNS depressant drug effect absent (if indicated, toxicology screen. If barbiturates given-serum level must be <10 ug/ml) d. No evidence of residual paralytics (train of four 4:4) e. No evidence of severe metabolic disturbance able to cause central nervous system depression (glucose, Na, PaCo2) Temp SBP f. Normothermia(>36 degrees C) g. Systolic BP > or equal to 100 mmHg h. No spontaneous respirations 2. Examination (all must be checked) a. Pupils nonreactive to bright light b. Absent corneal reflex c. Oculocephalic reflex absent (do not perform if c-spine precautions) d. Oculovestibular reflex absent e. No facial movements to noxious stimuli f. Absent gag and cough reflex g. Absence of motor response to noxious stimuli in all 4 limbs (spinal reflexes permissable) 3. Apnea testing (all must be checked) a. Patient is hemodynamically stable b. pre-oxygenate with 100% FiO2 for >= 10 minutes c. Obtain baseline ABG d. Adjust ventilator PaCo2 as close to 35-45 mmHg as possible e. Disconnect ventilator f. Provide oxygen via T-piece at 100% O2 g. Spontaneous respirations absent h. ABG drawn at 8-10 minutes i. Patient reconnected to ventilator j. PCo2 >= 60 mmHg or 20 mmHg rise above baseline value k. Apnea test: Posive Aborted Inconclusive 4. Ancillary Tests (recommemnded if clinical exam cannot be fully performed or apnea test aborted) a. Cerebral Arteriography c150910 b. EEG c. Radionucliotide CBF d. TCD or ICP equal to MAP Page 4 of 6 Determination of Death by Neurologic Criteria (Brain Death) PATIENT IDENTIFICATION LABEL University of Colorado Hospital BRAIN DEATH DETERMINATION DOCUMENTATION NOTE: The patient must be examined in this hospital during treatment of potentially correctable abnormalities. The examining physician will initiate each component of the exam and where appropriate, document supporting laboratory or examination data. If a component of the exam is not or cannot be done, please document. THE EXAMINING PHYSICIAN MUST DOCUMENT THE DATE AND TIME OF THE EXAMINATION. RESULTS OF EXAM MUST BE DOCUMENTED FOR ALL OF SECTIONS A, B, AND C AND ACCORDING TO GUIDELINES FOR SECTION D. EXAM Date : EXAM Time: Have reasonable efforts been made to notify patients’ family or decision maker that a determination of death based on cessation of brain function will be completed? Yes A. No Evidence of/Cause of Reversible CNS Depression 1. Core temperature must be greater than 360 Celsius. Record temperature Temp ______ 2. Record no evidence of severe metabolic perturbations that could potentiate central nervous system depression. Consider glucose, Na, creatinine, PaCO2, SaO2. No evidence 3. No CNS depressant drugs or paralytic agents given a minimum of 2-hours prior to exam. Record no evidence of pharmacological perturbations within 2-hours. Does the literature say this somewhere? If we are doing TOF and measuring pentobarb levels, does this timeframe matter? 4. Absence of hypotension (SBP greater than 90 mm Hg or MAP greater than 60 mm Hg). Record blood pressure. No evidence B/P ______ B. Absence of Cortical Function 1. No motor response to any stimuli (excluding spinal reflex) No response 2. No eye opening to any stimuli. No response 3. No verbal response to any stimuli. No response C. Absence of Brain Stem Reflexes and Responses **Physician must perform all 4 of the tests listed below. ** 1. Pupils non-reactive to strong light. Reflex absent 2. Absent corneal reflexes Reflex absent 3. Absent response to upper and lower airway stimulation, such as pharyngeal and endotracheal suctioning. Reflex absent 4. Absent ocular response to irrigation of the ears with 50 mL of ice water (no ocular cephalic reflexes) Reflex absent D. Document Confirmatory Test Utilized (minimum of 1) 1. Apnea Test: (with physician present) PaCO2 at start of test PaCO2 at end of test pH at end of test Other confirmatory tests are not required if a clinical exam including an apnea test is done. If an apnea test is not done as part of the clinical exam, one of the following confirmatory tests is required: □ EEG □ Cerebral arteriography 2. Other Test(s): □ Transcranial Doppler or ICP is equal to MAP □ Radionuclide CBF Having considered the above findings, I hereby certify brain death pronounced by: Attending Physician Signature ______________________________ Date_______________ Name Printed ____________________________ UPI#__________ Time _______________ MED 90304 E/-(05/07) c150910 Page 5 of 6 Determination of Death by Neurologic Criteria (Brain Death) References: 1. Greer, David M., Varelas, Panayiotis N., Wijdicks, Eelco F.M., Wijdicks, Shamael Haque. (2010). Variability of brain death guidelines in leading US neurologic institutions. Neurology, (70), 283-289. ( LOE 4). 2. Colorado Revised Statutes, Volume 4, Title 12 (May 21, 1997). § 12-36-136 Determination of death. (Retrieved from:?) (LOE?) 3. Ducrocq, X., Braun, M., Debouverie, M., Junges, C., Hummer, M. and Vespignani, H. (1998). Brain death and transcranial doppler: experience in 130 cases of brain dead patients. Journal of the Neurological Sciences, 160, 41-46. LOE 3) 4. Peiffer, K.M.Z. (2007). Brain death and organ procurement. AJN, 107, 3, 58-67. (Level VI) 5. Manno, E.M., & Wijdicks, E.F.M. (2006). The declaration of death and withdrawal of care in the neurologic patient. Neurologic Clinics, 24, 159-169 (LOE 5). 6. Wijdicks, Eelco F.M., Varelelas, Panayiotis N., Groneseth, Gary S., Greer, David M. (2010). Evidence-based guideline update: Determining brain death in adults: Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology, 74, 19101918. LOE 4). 7. Yee, Alan H., Mandrekar, Jay, Rabinstein, Alejandro A., Wijdicks, Eelco F.M. (2010). Predictors of apnea test failure during brain death determination. Neurocritical Care Society, online publication: 09 March 2010. (LOE 5). 8. Llompart-Pou, J.A., Abadal, J.M., Velasco, J., Homar, J., Blanco, C., Ayestaran, J.I., PerezBarcena, J. (2009). Contrast-enhances transcranial color sonography in the diagnosis of cerebral circulatory arrest. Transplantation Proceedings, 41, 1466-1468. (LOE 4) c150910 c150910 Page 6 of 6