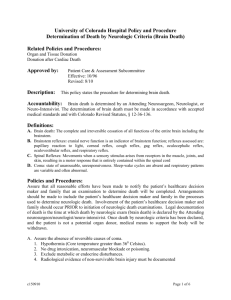
Appendix A: Detailed Recommendations for Brain Death Examination
advertisement

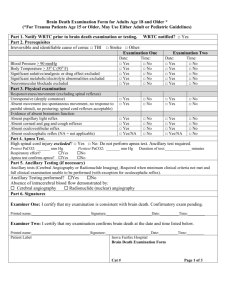
Interdisciplinary Clinical Practice Manual,Medical Legal, Brain Death, Determination of Death by Neurologic Criteria, MEL005 Effective Date: 07/05/2014 Page 1 of 2 Appendix A: Detailed Recommendations for Brain Death Examination Appendix A: Detailed Recommendations for Brain Death Examination A. B. C. Motor and Autonomic Assessment 1. For the determination of brain death, an intense noxious stimulus may be used to demonstrate absence of response, but it is not acceptable to use instruments (e.g. clamps, hemostats), or other objects that would physically harm the patient. Appropriate stimuli include pressure on the supraorbital ridge, stylomastoid process, clavicle, sternum, nailbeds, or pinching the trapezius. Flexion, extension, and localizing responses must be absent. 2. Movements of spinal cord origin occasionally occur, and may be difficult to distinguish from cortically-mediated movement. Triple flexion responses, deep tendon reflexes, superficial abdominal reflexes, and the Babinski sign may all occur in brain dead patients. If motor responses are equivocal in nature, it is advisable to repeat the examination after an appropriate interval, or to seek a second opinion from another physician qualified to determine brain death. 3. There must be no discernible increase in heart rate or blood pressure in response to a noxious stimulus. Brainstem Reflexes 1. Pupillary constriction to light (Cranial nerves II and III). Pupil diameter must be mid-range or dilated and responsiveness to light must be absent bilaterally. It is important to determine if the patient had preexisting pupillary abnormalities (e.g., secondary to eye surgery). 2. Oculocephalic reflex (Doll’s eyes test; cranial nerves III, IV and VI) is assessed by holding the eyes open and gently rotating the head from side-to-side. If there is no movement of the eyes relative to the head, the reflex is absent. This test must not be performed if there is a known or potential fracture or instability of the cervical spine. 3. Vestibulo-ocular reflex (Cranial nerves III, VI and VIII). Determine that the ear canals are clear of obstruction, and the tympanic membranes are not ruptured. Slowly instill 60 cc of ice water into each ear canal separately (use a large syringe connected to a peripheral IV catheter). If there is no movement of the eyes, the reflex is absent. This test must not be performed if there is injury to the tympanic membrane. 4. Corneal reflex (Cranial nerves V and VII) can be tested with a cotton swab applied to the corneal surface. Care must be taken to stimulate the cornea directly, and not the sclera. If there is no eyelid contraction (including absence of subtle lower lid movement), the reflex is absent. 5. Facial grimace (Cranial nerves V and VII) can be tested by pressing on the supraorbital ridge. Observation for facial grimace must also occur during application of painful stimuli to the limbs or torso when assessing motor response. If there is no facial grimace, the reflex is absent. 6. Cough reflex (Cranial nerves IX and X). The carina is stimulated by a suction catheter passed through the endotracheal tube. If there is no cough, the reflex is absent. Side-to-side or up-and-down jiggling of the ET tube is an insufficient stimulus for the brain death examination. 7. Gag reflex. A cotton swab or tongue depressor is used to gently stimulate the soft palate or posterior oropharynx. If there is no gag, the reflex is absent. Apnea Test 1. The goal of the apnea test is to allow the PaCO2 to rise, or the pH to decline, to levels that would cause respiration to occur. The absence of any respiratory effort and a concomitant rise in PaCO2 suggest severe damage to brainstem respiratory centers. The apnea test is necessary but not sufficient for the clinical diagnosis of brain death. The apnea test can result in significant physiological perturbations including hypoxia, hypotension, and arrhythmias. 2. Because the apnea test requires meticulous observation of the absence of respiratory effort, and because of the potential complications of the apnea test, the physician determining brain death must remain at the bedside and observe the patient for the duration of the apnea test. 3. Prerequisites for the apnea test are the same as for the brain death examination (see V.4.D.), but with the addition of: a. An arterial blood gas must be obtained immediately prior to the test. It must demonstrate normocapnea (PaCO2 35-45 mmHg), or in patients with chronic hypercapnic respiratory failure, a normal pH (7.35-7.45). Blood gas must also demonstrate a sufficient degree of oxygenation (PaO2 > 60 mmHg). Pre-oxygenation at FiO2 1.0 can help to delay or prevent hypoxia during the test. b. Adequate physiologic monitoring, including continuous arterial blood pressure measurement, ECG, and pulse oximetry. c. ICU and laboratory staff and necessary equipment for serial arterial blood gases. Interdisciplinary Clinical Practice Manual,Medical Legal, Brain Death, Determination of Death by Neurologic Criteria, MEL005 Effective Date: 07/05/2014 Page 2 of 2 Appendix A: Detailed Recommendations for Brain Death Examination 4. 5. 6. 7. The patient is disconnected from the ventilator, and a canula with oxygen 4-10 L/min (0.5-2 L/min in children) is placed in the endotracheal tube and advanced to the level of the carina. The patient must be continuously monitored throughout the test for evidence of respiratory effort. Arterial blood gas must be collected 5 min after disconnection of the ventilator and repeated at 5 min intervals. Depending on the patient’s basal metabolic rate, the test can take as long as 15-20 min. The apnea test is positive if: a. No spontaneous breathing is appreciated AND b. The PaCO2 rises to >/=60 mmHg OR c. The PaCO2 increases by >/=20 mmHg above the pre-test value, provided the pre-test PaCO2 approximates the patient’s pre-morbid baseline PaCO2 (the latter criterion is especially relevant in patients with chronic hypercapnia). The apnea test must be terminated and the ventilator reconnected if: a. There is any respiratory effort, including cough or gasp. If this occurs, ventilatory drive is present and the neurologic criteria for death are not met. b. Hypotension (systolic blood pressure <90 mmHg) occurs which cannot be rapidly corrected with fluids or vasopressors, or hypoxia (SaO2 <90%) occurs. If the apnea test is interrupted for these reasons, obtain an arterial blood gas before reconnecting the ventilator; if the PaCO2 is neither >/=60 mmHg, nor >/= 20 mmHg above baseline, then the apnea test is negative and a confirmatory test must be obtained.