Declaration of Brain Death
advertisement

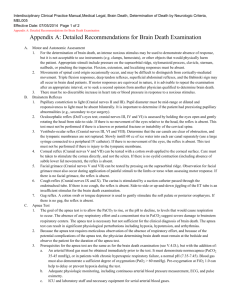
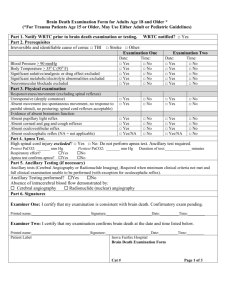
Determination of Brain Death Donn Dexter, MD, FAAN Douglas T. Miller Symposium April 29, 2011 Disclosures • Full time physician at Luther-Midelfort Mayo Heath System, Eau Claire, Wisconsin. • No financial relationships or interests that pertain to organ donation. Outline • What is Brain Death? • How Do You Declare Brain Death? – Clinical Evaluation – Neurologic Evaluation – Apnea Test – Ancillary Tests • Conclusion Determination of Brain Death • Uniform Determination of Death Act • • (UDDA). An individual who has sustained either: 1) irreversible cessation of circulatory and respiratory function or 2) irreversible cessation of all function of the entire brain, including brain stem, is dead. A determination of death must be made with acceptable medical standards. Determination of Brain Death • The American Academy of Neurology (AAN) delineated the medical standards for brain death in 1995. • This practice parameter was reviewed in 2010 (Neurology 74, June 8, 2010). Determination of Brain Death • Question for the 2010 AAN review: Are there patients who fulfill the criteria of brain death who recover brain function? • In adults, the recovery of brain function has not been reported after clinical declaration of brain death using the 1995 AAN brain death criteria. Determination of Brain Death • Determination of Brain Death – 4 Steps 1) Establish irreversible and proximate cause of coma. 2) Achieve normal core temperature. 3) Achieve normal systolic blood pressure. 4) Perform neurologic examination. The Clinical Evaluation • Establish Irreversible and Proximate Cause of Coma – Usually obvious. – Exclude drugs (including alcohol above legal limit). – No recent or persistent neuromuscular blocking agents (train of 4 twitches to nerve stimulation). – No severe electrolyte, acid-base, or endocrine disturbance (ABGs, lytes, chem panel). The Clinical Evaluation (cont.) • Achieve Normal Core Temperature – Core body temperature > 36 degrees C. – Important for apnea test. – Warming blanket and warmed IV fluids may be required. The Clinical Evaluation (cont.) • Achieve Normal Systolic Blood Pressure – Neurologic examination usually reliable with systolic BP > 100 mmHg. – UW-OPO requires systolic BP > 100 mmHg. – May require vasopressors to maintain adequate BP (dopamine and neosynephrine often preferred). The Clinical Evaluation (cont.) • Perform Neurologic Examination – One examination is sufficient. – Examiner should be intimately familiar with brain death criteria. – Most commonly a critical care specialist, neurologist, or neurosurgeon. – Varies by state. Outside WI check with state statute. The Neurologic Examination • Coma – No evidence of responsiveness. – No eye opening to noxious stimuli. – No motor response to noxious stimuli other than spinally mediated reflexes (may require expertise to distinguish). The Neurologic Examination (cont.) • Absence of Brainstem Reflexes – No pupillary response to bright light (typically fixed @ 4-9 mm). – Absent corneal reflex. – Absent facial muscle movement to noxious stimulus. – Absent pharyngeal and tracheal reflexes (gag and deep suction). The Neurologic Examination (cont.) • Absent Brainstem Reflexes (cont.) – Absent eye movements to oculocephalic testing (doll’s eyes test); integrity of cervical spine must be certain. – Oculovestibular testing (cold water calorics) – Head of bed 30 degrees, 50 mL ice water irrigation of each patent ear canal with 5 minutes observation and 5 minutes between tests. The Apnea Test • Preconditions – Normothermia. – Systolic BP > 100 mm Hg. – Euvolemia (positive fluid balance). – Eucapnia (PaCO2 35-45 mmHg). – No evidence for CO2 retention (COPD, severe obesity, severe OSA). The Apnea Test (cont.) • Preoxygenate for 10 minutes to PaO2 >200 mm Hg. • Reduce ventilation frequency to 10 bpm and PEEP to 5 cm H2O. • If pulse oximetry remains > 95%, check baseline ABG. • Disconnect ventilator and preserve oxygenation with 100% O2 @ 6-10 lpm via catheter through the ET at level of carina. The Apnea Test (cont.) • Watch closely for respiratory movements (abdominal or chest excursions). • If no respiratory efforts, draw ABGs at 3-5 minutes and again at 7-10 minutes. • If arterial PaCO2 is 60 mm Hg or greater or if >20 mmHg over baseline, the test is positive. • If inconclusive, may extend to 10-15 minutes if clinically stable. The Apnea Test (cont.) • Abort Apnea Test for: – Spontaneous respiratory effort. – Significant cardiac ectopy. – Pulse oximetry <90%. – Systolic blood pressure < 90 mmHg. Ancillary Testing • EEG, TCD, CTA, MRI/MRA, cerebral angiography, and nuclear scans have all been used to confirm brain death. • Used when standard testing impossible or inconclusive (i.e. aborted apnea test). • EEG, cerebral angiography, and nuclear scan preferred. Documentation • Follow checklist closely! • Time of death is the time PaCO2 reached target. • If apnea test aborted, the time of death is the time ancillary test is interpreted. Conclusion • Have a clear and available protocol for the determination of brain death at your institution (UW-OPO has a good one). • Review it regularly; test it formally. • Follow it closely.