Brain Death Simulation Workshop November 8
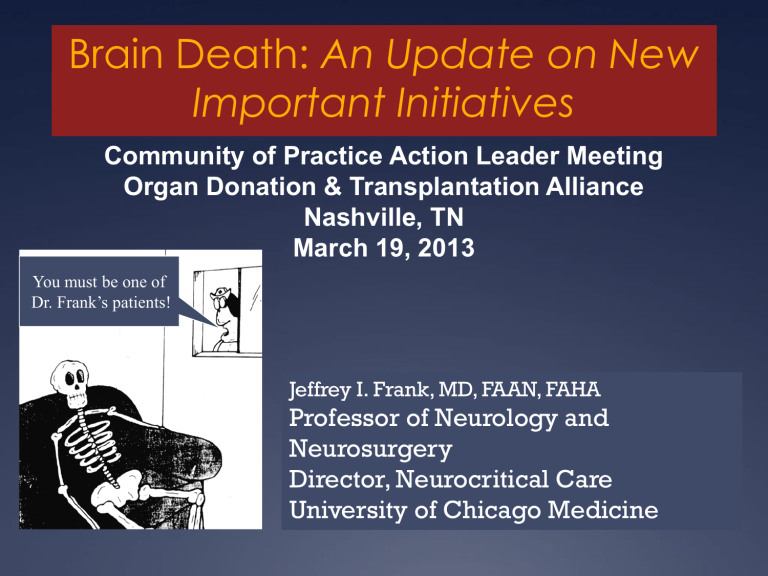
Brain Death: An Update on New
Important Initiatives
Community of Practice Action Leader Meeting
Organ Donation & Transplantation Alliance
Nashville, TN
March 19, 2013
You must be one of
Dr. Frank’s patients!
Jeffrey I. Frank, MD, FAAN, FAHA
Professor of Neurology and
Neurosurgery
Director, Neurocritical Care
University of Chicago Medicine
Disclaimer
I am NOT a passionate about organ donation advocate
My presence at this meeting IS NOT about enhancing organ donation
My passion and presence IS about my role in:
Improving contemporary understanding of brain death
Assuring integrity in brain death diagnosis and patient/family management through better education of physicians and nurses, and better uniformity of policies
Implications for organ donation but it NOT ABOUT organ donation (ODMT: DDWG)
Pre-Ventilator Era
Any process that arrested breathing led to asystole and a cold, blue corpse
Apnea Asystole
1928
Ventilator Era (1960’s)
?
1952 1972
Now patients with severe brain dysfunction were on ventilators!
Spectrum of Brain Injury
With Mechanical Ventilation
Moderate:
Awake or drowsy with disability
Major:
Coma with some brain function
Extreme:
No discernible brain function
Required
Definition
Brain Death History
Harvard
(1968)
“Irreversible Coma”
No brainstem reflexes
“Flat” EEG
Proposed brain death
NIH Collaborative Study
(1977)
Defined the futility of brain death
President’s Commission Report
(1980)
Affirmed the validity of brain death
Proposed guidelines on how to approach brain death diagnosis
Declaration of Death Act
Uniform Declaration of Death Act (1980)
Basis for Brain Death Law
Dead if irreversible cessation of either:
–
–
Circulatory and respiratory functions, or
All functions of the entire brain, including brainstem (brain death)
BRAIN DEATH IS THE IRREVERSIBLE CESSATION OF
WHOLE BRAIN FUNCTION
(HEMISPHERES AND BRAINSTEM)
1995
AAN Creates Practice Parameter:
Guideline
Brain Death in the U.S.
1920
Iron Lung
Invented
Harvard
Report
1965
Modern mechanical ventilation (critical care)
Transplant
Reality
NIH
Study
President’s
Commission
Report
UDDA
CT Scanner
Invented
2012
Societal Evolution and Acceptance (death with a heart beat)
Irreversible cessation of whole brain function = Death
Real mechanism of death
Can be reliably diagnosed
Paradigm Shift
Brain Death Today
Mechanism of death: Widely accepted
Diagnosis: Important; Independent of OD
Contemporary Imperative
Mandatory, accurate, and expeditious diagnosis
Respect for process
Proactive management of physiology
Thoughtful interaction with family/surrogates
Thoughtful sequencing of involvement of health care teams and OPOs
Profound variability in policy and practice
Guideline performance
Pre-clinical testing
Clinical examination
Apnea testing
Ancillary testing
Physicians Responsible for
Brain Death Diagnosis
11%
36%
43%
10%
Intensivist Primary Attending No mention N/NS
Preclinical Testing:
Compliance with AAN Guidelines
100%
90%
89%
80%
70%
60%
50%
40%
30%
20%
10%
0%
81%
72% 71%
63%
55%
45%
42%
Clinical Exam:
Compliance with AAN Guidelines
100%
100%100% 97% 95%
87% 87% 87%
90% 82%
80%
30%
20%
10%
0%
70%
60%
50%
40%
42%
27%
18%
100%
90%
80%
70%
60%
50%
40%
30%
20%
10%
0%
Apnea Testing:
Compliance with AAN
Guidelines
87% 87%
76% 71%
66%
55%
48%
39%
16%
Ancillary Testing
100%
90%
80%
70%
60%
50%
40%
30%
20%
10%
0%
66%
84%
33%
42%
21%
74%
29%
66%
21% 24% 18% 24%
Variability in BD Determination Practice:
a review of 226 brain dead organ donors (2011)
Claire Shappell MS2, Jeffrey Frank MD
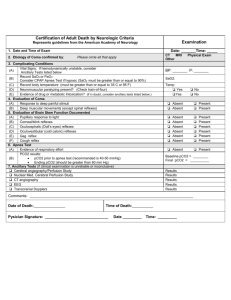
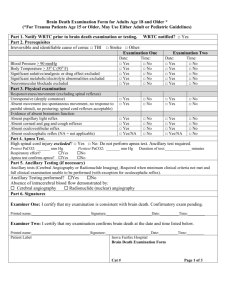
AAN Approach to Determining
Brain Death
Part 1
Coma
Known Cause
Irreversible
“Pre-Requisites”
Neuroimaging compatible
Part 2
Absent
Reflexes
Pupillary
Doll’s Eyes
Cold Water Calorics
Corneal
Gag
Cough
Motor
Part 3
Apnea
Loss of respiratory drive
Specific method of testing for apnea
Rise in CO
2 with no breaths observed
Ancillary Tests
Sometimes, Part 4
Nuclear Medicine Blood Flow Study
Electroencephalography (EEG)
CT Angiography
Conventional Angiography
Required ONLY if clinical examination or apnea testing cannot be fully performed
Results: Overview and Part 1
Total Patients
Age, mean (SD), y
Male Sex, No. (%)
Cause of Death, No. (%)
Intracranial Hemorrhage
Trauma
Anoxia
Unknown
Ischemic Stroke
Other
226
46 (16)
115 (51)
95 (42)
59 (26)
44 (19)
9 (4)
8 (4)
8 (4)
100%
Results: Brain Stem Reflexes
99%
96% 95% 94%
80%
80%
69%
66%
60%
40%
20%
0%
Pupillary Corneal Motor Gag Doll's Eyes Cough Calorics
Mean # of reflexes documented: 6 ±1.2
All reflexes documented (7 of 7): 101 (44.7%)
100%
80%
60%
40%
20%
0%
Apnea and Ancillary Studies
Apnea Test
Completed
Aborted
Not Performed
# Donors (%)
162 (71.7)
12 (5.3)
46 (20.4)
35%
NM
28%
EEG
13%
CTA
2%
TCD
2%
Angio
8%
Other
Putting it all together
81%
All Brain Dead
Organ Donors n=226
Coma
Cause Known n=217
Normothermic
(≥36°C) n=184
Reflexes Absent
± Redundant n=157
Apnea Test OR
Ancillary Study n= 151
Conclusions
36.7% documented adherence to all AAN practice recommendations for brain death diagnosis
66.8% documented adherence to AAN recommendations with weaker brain stem reflex standard (
± redundant reflexes)
At least 1/3 of brain death determinations do NOT have documentation of necessary features of brain death
What are we doing to improve the field?
Educational/training endeavors
Web-based training: Acute Review (CCF, Prpvencio)
Webinars: Frank, Greer, Goldenberg, Provencio
Simulation training:
Basic training (Yale, Greer)
“Champions”: Training Leaders (UofC, Frank, Goldenberg)
Brain Death Simulation Training
November 12, 2012
Second International Brain Death
Simulation Workshop: Training
Future Leaders
Clinical Cases
Intoxication
Dummy
Simulation
Station
DDNC
BD
Physiological
Management
Station
Ancillary Tests
Station
Involuntary
Movements
Station
MD/Family
Interaction
Station
Isolated BS
Injury
Post CA w/o CE
Apnea Test
Grade V SAH
Catastrophic
Brain Injury
What are we doing to improve the field?
Educational/training endeavors
Web-based training: Acute Review
Simulation training: Basic training
“Champions”: Training Leaders
Creation of a national/international standard
Re-evaluate protocols since the 2010 AAN Practice
Parameters (WE NEED YOUR HELP)
Lobby at a national level for uniformity
Brain Death Ethics Subcommittee of NCS
Taking leadership/ownership regarding Brain Death
Education, Advocacy, Policy
Adaptation to Technology
End-Stage
Cardiomyopathy
VAD
Insertion
Perioperative
MI and
Cardiac Arrest
Continuous Flow
Ventricular Assist
Device
Death of Heart
Muscle: Permanent
Asystole
Post-Event Scenario
• Permanent asystole
• Maintained perfusion through VAD
• Brain with continued blood flow
•Systemic perfusion
•No heart beating
Heart Stops = Dead Brain Death = Dead
Heart stops but device maintained systemic perfusion
= Alive
Summary
Brain Death is an Important Diagnosis
Shift in accountability and responsibility for the integrity of brain death diagnosis, patient/family management, and policies/advocacy
Educational efforts
Academic efforts
Policy change
Better uniformity
“Growth means change and change involves risk, stepping from the known to the unknown”