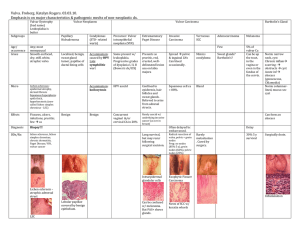
Epidemiology & Pathogenesis Clinical Dermoscopy Histo Progn
advertisement
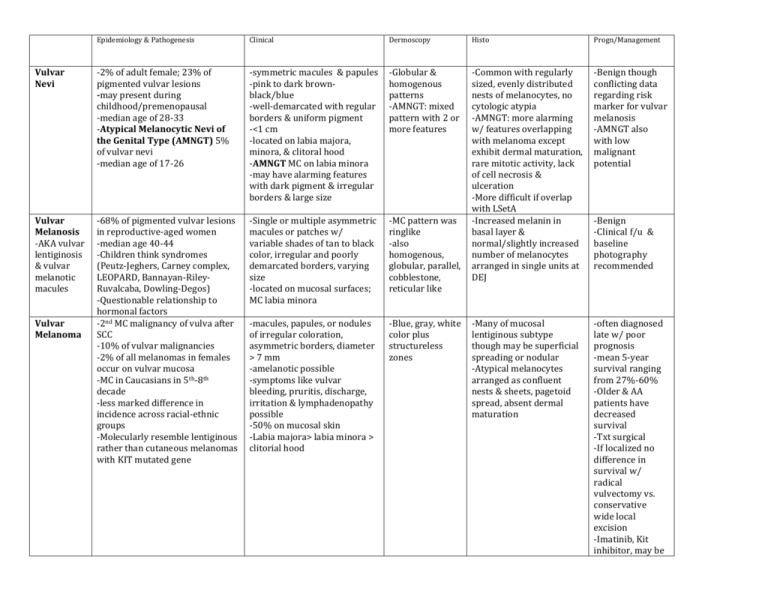
Epidemiology & Pathogenesis Clinical Dermoscopy Histo Progn/Management Vulvar Nevi -2% of adult female; 23% of pigmented vulvar lesions -may present during childhood/premenopausal -median age of 28-33 -Atypical Melanocytic Nevi of the Genital Type (AMNGT) 5% of vulvar nevi -median age of 17-26 -symmetric macules & papules -pink to dark brownblack/blue -well-demarcated with regular borders & uniform pigment -<1 cm -located on labia majora, minora, & clitoral hood -AMNGT MC on labia minora -may have alarming features with dark pigment & irregular borders & large size -Globular & homogenous patterns -AMNGT: mixed pattern with 2 or more features -Benign though conflicting data regarding risk marker for vulvar melanosis -AMNGT also with low malignant potential Vulvar Melanosis -AKA vulvar lentiginosis & vulvar melanotic macules -68% of pigmented vulvar lesions in reproductive-aged women -median age 40-44 -Children think syndromes (Peutz-Jeghers, Carney complex, LEOPARD, Bannayan-RileyRuvalcaba, Dowling-Degos) -Questionable relationship to hormonal factors -2nd MC malignancy of vulva after SCC -10% of vulvar malignancies -2% of all melanomas in females occur on vulvar mucosa -MC in Caucasians in 5th-8th decade -less marked difference in incidence across racial-ethnic groups -Molecularly resemble lentiginous rather than cutaneous melanomas with KIT mutated gene -Single or multiple asymmetric macules or patches w/ variable shades of tan to black color, irregular and poorly demarcated borders, varying size -located on mucosal surfaces; MC labia minora -MC pattern was ringlike -also homogenous, globular, parallel, cobblestone, reticular like -Common with regularly sized, evenly distributed nests of melanocytes, no cytologic atypia -AMNGT: more alarming w/ features overlapping with melanoma except exhibit dermal maturation, rare mitotic activity, lack of cell necrosis & ulceration -More difficult if overlap with LSetA -Increased melanin in basal layer & normal/slightly increased number of melanocytes arranged in single units at DEJ -macules, papules, or nodules of irregular coloration, asymmetric borders, diameter > 7 mm -amelanotic possible -symptoms like vulvar bleeding, pruritis, discharge, irritation & lymphadenopathy possible -50% on mucosal skin -Labia majora> labia minora > clitorial hood -Blue, gray, white color plus structureless zones -Many of mucosal lentiginous subtype though may be superficial spreading or nodular -Atypical melanocytes arranged as confluent nests & sheets, pagetoid spread, absent dermal maturation -often diagnosed late w/ poor prognosis -mean 5-year survival ranging from 27%-60% -Older & AA patients have decreased survival -Txt surgical -If localized no difference in survival w/ radical vulvectomy vs. conservative wide local excision -Imatinib, Kit inhibitor, may be Vulvar Melanoma -Benign -Clinical f/u & baseline photography recommended promising