Irritant
advertisement
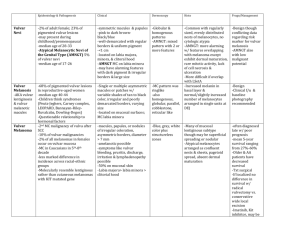
Evaluation and Medical Management of Vulvar Dermatoses Katherine “Casey” Monahan, FNP-C, Dermatology Providence Little Co. of Mary Dermatology & Laser Center Types • Dermatitis – acute inflammation • Contact dermatitis • Dermatoses – chronic inflammation • Lichen simplex chronicus • Lichen sclerosus • Lichen planus History • Specific areas to address include: • Major complaints • Hygienic practices • Types of clothing • Medications • Personal and family history • Sexual history Physical Examination & Diagnostics • • • • • Inspect the entire vulvar and perianal area with good lighting Inspect the mouth Swabs for microbiology Skin biopsy Patch testing Exogenous (Contact) Dermatitis • Vulvar dermatitis (eczema) – the most common vulvar dermatosis • Two types of contact dermatitis • Allergic (20% of cases) • Irritant (80% of cases) Contact Dermatitis • • • • Vulvar tissue more permeable than exposed skin Typically, allergens are new exposures Allergic reactions require prior exposure to a product Irritants cause an immediate response, whereas allergic reactions occur 12 to 72 hours after exposure Contact Dermatitis • Signs and Symptoms • Redness, swelling, and scaling of the labia minora • Superficial fissures • Pain and burning at rest • Introital dyspareunia • Generalized pruritus less common Contact Dermatitis Contact Dermatitis • Allergens • Fragrances, preservatives, topical medications, and rubber • Propylene glycol • Irritants • Anti-fungal, anti-bacterial, and steroidal creams/ointments • Preservatives, stabilizers, and delivery vehicles in drugs, as well as the drugs themselves Contact Dermatitis Irritants Allergens • Bubble baths • Chlorhexidine • Baby wipes • Perfume • Talcum powder • Neomycin • Urine • Nickel • Feces • Nail polish • Deodorants • Latex • Sanitary protection • Spermicides • Soaps • Benzocaine Contact Dermatitis • Management • Identify and eliminate causative agent(s) • Replace all known irritant agents with hypoallergenic moisturizing preparations • Local measures • Oatmeal colloidal soaks • Ice packs • Mild steroidal ointment in petroleum • Aqueous 4% Xylocaine solution Contact Dermatitis Lichen Simplex Chronicus (“LSC”) • Occurs in chronic cases of dermatitis, resulting from rubbing and scratching • Characterized by skin lichenification and excoriation, together with pigmentary abnormalities • Accentuation of skin lines/markings • Leathery texture LSC LSC • Management • Goal: cessation of pruritus • Avoid scratching • High-potency steroid cream/ointment initially, then medium- to lower-strength topical steroids • Occlusion of medium-potency steroids • Intralesional kenalog injections (5 – 10mg/ml) • Unna boot Lichen Sclerosus Lichen Sclerosus et Atrophicus (“LS&A”) • Most common vulvar dermatosis/disease • Chronic, inflammatory, autoimmune disease of the skin and mucosae, preferentially affecting the vulva • Most common among post-menopausal women (up to age 90 yrs.); females predominately • May affect children (from age 5 mos.) and young adults • If untreated, can result in fusion around the clitoris (phimosis), atrophy and splitting of the vestibule, severe narrowing of the vaginal orifice, and, rarely, vulvar cancer (squamous cell carcinoma (“SCC”)) LS&A • Signs • Atrophy • White patches surrounded by erythematous or violaceous halos • Lesions may coalesce into large atrophic erosions, making the skin smooth, wrinkled, soft, and white • Excoriations or superficial fissures • *characteristic signs that help distinguish LS&A * LS&A • Signs • Thickened areas • Vulvar and perineal involvement leads to “figure-eight” or “hourglass” shape around the anus • Obliteration of architecture with loss of labia minora, clitoral hood, and urethral meatus • Labial stenosis or fusion LS&A LS&A LS&A • Symptoms – mean duration 99 months • Intense pruritus • Soreness • Burning • Dyspareunia LS&A • Management • Biopsy • Clobetasol ointment = drug of choice • Effective in 90% of patients with reversal of epidermal atrophy LS&A • Refractory/Severe Cases • Cortisone injections • Oral retinoid therapy and topical tretinoin • Maintenance with testosterone ointment and progesterone cream • Surgery rarely indicated Lichen Planus • Chronic, inflammatory, autoimmune disease involving: • Glabrous skin (flexor surfaces of arms and legs) • Hair-bearing skin and scalp • Nails • Mucous membranes of the oral cavity and vulva • >70% of patients between the ages of 30 and 60 years Lichen Planus • Vulvo-vaginal-gingival syndrome: involves vulva and vagina with gingivitis • Oral lesions may precede or follow vulvovaginal lesions by months or years or may be simultaneous • Vaginal mucosa involved in two-thirds of cases • In one-third of cases, reticulate buccal involvement • 10% have concurrent cutaneous lesions Lichen Planus • Vulvovaginal signs • Rarely presents as the classic widespread shiny, violaceous, pruritic, flat-topped papules • Erosive/ulcerative form most common presentation in mucous membranes • Mucosal: white reticulate or lace-like changes (Wickham’s striae) or erosions • Vulvar: erythematous erosions with narrow rim of white reticulation • Vaginal: glazed erythema, easy friability Lichen Planus • Vulvovaginal symptoms • Pruritus on hair-bearing vulvar skin • Severe burning pain in the vestibule or vagina Lichen Planus • • • • • • May be subtle and mistaken for vulvodynia Typically, morphology similar to vulvar lichen sclerosus Late scarring with loss of labia minora and clitoral hood Adhesion formation in upper part of vagina Total vaginal obliteration Erosive mucosal cases considered pre-malignant Lichen Planus Lichen Planus Lichen Planus Lichen Planus Lichen Planus Lichen Planus • Management • Biopsy: histological evaluation superior to direct immunofluorescence • Topical and/or intravaginal steroid = first-line therapy Lichen Planus • Vulvar management • Clobetasol or another high-potency topical steroid ointment BID • Long-term maintenance with low or mid-potency topical steroid ointment • Calcineurin inhibitors: tacrolimus (Protopic) and pimecrolimus (Elidel) cream BID or suppository QHS • Oral hydroxychloroquine (Plaquenil), cyclosporine, azathioprine (Imuran), etanercept (Enbrel), methotrexate Lichen Planus • Vaginal management • Anusol hydrocortisone suppositories • Vaginal dilation • Surgery