Vulvar Vestibulitis Subtype

VULVODYNIA
Clinical Aspects and Research Initiative
Gloria A. Bachmann, M.D.
Nidhi Gupta, M.D.
Women’s Health Institute
UMDNJ-Robert Wood Johnson Medical School
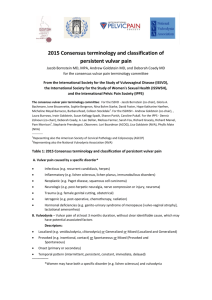
Defining Vulvodynia
The International Society for
Study of Vulvovaginal Diseases
(ISSVD) defines vulvodynia as
‘chronic vulvar discomfort, characterized by the woman’s complaint of burning, stinging, irritation or rawness’
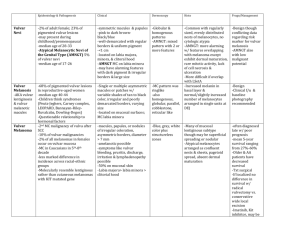
Types of Vulvar Pain
PAIN from an
IDENTIFIABLE
ETIOLOGY
VULVODYNIA
Vulvar
Vestibulitis
Subtype
(provoked)
Dysesthetic
Vulvodynia
Subtype
(unprovoked)
Pain from an
Identifiable Etiology
Infections such as chronic vulvovaginitis caused by Candida or other pathogens
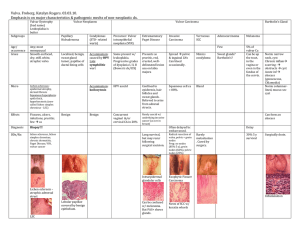
Dermatoses and Dermatitis that involve the vulva such as Lichen
Sclerosus, Lichen Planus, irritants and allergic dermatitis
Vaginismus
Vulvodynia:
Vulvar Vestibulitis Subtype
1.
2.
3.
Friedrich’s criteria diagnostic
:
1. Severe pain on vestibular touch or attempted vaginal entry.
2. Tenderness to pressure localized within the vulvar vestibule
3. Physical findings confined to vestibular erythema of various degrees
Pain is provoked and localized
Commonly seen in women aged 50 years or less
Vulvodynia:
Dysesthetic Vulvodynia Subtype
Pain is constant and may be felt beyond the confines of vulvar vestibule
Usually pain is unprovoked
Diagnosed mainly in women who are peri- or postmenopausal
Vulvodynia:
Prevalence Statistics
Harvard-based study (n=16,000) estimates a 16% life time prevalence *
UMDNJ-based study estimates:
21% prevalence of chronic
gynecologic pain
13.5% prevalence of vulvodyniatype pain
* Harlow BL, Stewart EG. A population-based assessment of chronic unexplained vulvar pain: have we underestimated the prevalence of vulvodynia?
J Am Med Women's Assoc 2003;58:82-88
Vulvodynia:
Demographics
Older data suggest the highest prevalence in white women
Accounts for 10 million doctor visits/year
Upwards of 14 million women are affected in their lifetime
Recent data suggest Hispanic women 80% more likely to have vulvar pain than other racial groups
Etiology:
Vulvar Vestibulitis Subtype
Prior vulvovaginal Candidiasis
Hypersensitivity to chemicals
Human Papilloma virus infection
High levels of urinary oxalates
Neurological dysfunction
Candida Etiology:
Vulvar Vestibulitis Subtype
In 1989 Ashman and Ott proposed cross reaction between Candida albicans antigens and self-antigen in vulvovaginal tissue
Affected tissue has locally elevated concentrations of inflammatory cells and pro-inflammatory cytokines
These suggest a hyper-immune response, possibly from persistent antigen from the
Candida
Proposed Etiologies:
Vulvar Vestibulitis Subtype
Calcium oxalate crystals in urine may act as irritant to the vulva
Reduced estrogen receptor
expression causing alteration in vulvar sensation *
CNS etiology, similar to other regional pain syndromes
* Eva LJ, MacLean AB, Reid WMN, et al. Estrogen
Receptor Expression in Vulvar Vestibulitis Syndrome.
Am J Obstet Gynecol 2003;189:1-4.
Proposed Inflammatory Etiology:
Vulvar Vestibulitis Subtype
An inflammatory event releases cytokines that sensitize nociceptors in the nerve fibers of the vulva *
Increased intraepithelial nerve endings in vestibulitis patients have been reported. Prolonged neuronal firing sensitizes neurons in dorsal horn of spinal cord, with subsequent abnormal interpretation as pain from touch **
Etiology: Dysesthetic
Vulvodynia Subtype
Etiology not definitively known
Childhood trauma and OCP’s possible contributors
Sympathetic pain loops caused by repeated irritation/trauma leads to continuous vulvar symptoms *
* Davis GD, Hutchison CV. Clinical Management of
Vulvodynia. Clinical Obstetrics and Gynecology
June 1999; 42(2):pp 221-233.
.
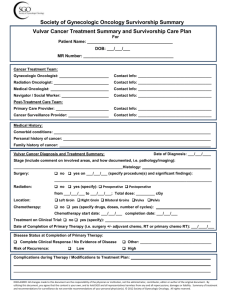
Vulvodynia:
Assessment of the Patient
OB/GYN history
Detailed pelvic exam to exclude pathology
Vaginal culture
(in selected cases)
Pap smear
Vulvodynia:
Assessment of the Patient
Vaginal pH
Urinanalysis for oxalate content
(select cases)
Biopsy of abnormal vulvar areas
Psychosocial assessment
Vulvodynia:
Assessment of Pain Intensity
Clinician Assessment:
Q–tip test
Vulvalagesiometer- A device developed at
McGill University for nominal scale vulvar pain measurement
*
Vulvar Algesiometer- Developed by
Curnow to quantify pain by nominal scale
**
* Pukall CF, Payne KA, Binik YM, Khalife S. Pain measurement in vulvodynia.
20,2003.
Journal of Sex and Marital Therapy . 29 Suppl 1:111-
** Curnow JS, Barron I, Morrison G., et al. Vulval algesiometer.
Med Biol Eng Comput 1996;34:266-9.
Vulvodynia:
Assessment of Pain Intensity
Patient Assessment:
McGill-Melzack Pain Questionnaire-
78 pain words grouped in 20 subclasses of 3-5 descriptive words *
Subclasses are grouped in four sections, sensory, affective, evaluative and miscellaneous.
Provides information on timeline, location and a quantitative measure of clinical pain.
Vulvodynia:
Differential Diagnosis
Exclude other pain causes:
1.
Vaginitis, Candida, urethritis, interstitial cystitis, Herpes,
Bartholin adenitis
2.
3.
4.
Vulvar Dermatoses and
Dermatitis such as eczema
Vaginismus, entry and deep dyspareunia
Atrophic Vulvo-Vaginitis
Vulvodynia:
Diagnosis
“Diagnosis made after thorough evaluation fails to identify pain etiology”
Vulvodynia: Management
Vulvar Vestibulitis Subtype :
Non-Pharmacologic
Pharmacologic
Surgical
Dysesthetic Vulvodynia Subtype :
Non-Pharmacologic-
Not recommended
Pharmacologic
Surgical-
Not recommended
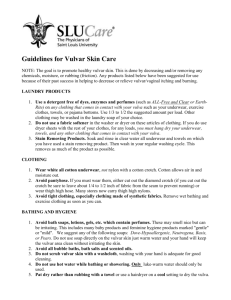
NonPharmacologic Management:
Vulvar Vestibulitis Subtype
Patient education and counseling
Physical therapy and biofeedback
Life-style modification
Application of ice and local anesthetics to the vulvar region as needed
NonPharmacologic Management:
Vulvar Vestibulitis Subtype
Low Oxalate Diet
Oxalate is a metabolic breakdown product from certain food types
Oxalates excreted in urine as crystals
Vulvar surface contact with oxalate crystals causes irritation and burning
Low oxalate diet (with calcium citrate supplementation) may be beneficial
NonPharmacologic Management:
Vulvar Vestibulitis Subtype
Calcium Citrate and the Low
Oxalate Diet
Degradation of vulvar collagen and hyaluronic acid also increase oxalate pool
Calcium citrate inhibits hyaluronidase and the release of oxalates and acts as a free radical scavenger *
1200 mg of calcium citrate daily aids in further reducing urinary oxalate levels **
Biofeedback:
Vulvar Vestibulitis Subtype
Surface electromyographic biofeedback data suggest persistent vulvar injury leads to chronic reflex pain, resulting in increased muscle tension *
Pelvic floor muscle instability may be present
If pelvic floor abnormalities present, physical therapy often beneficial
* Glazer H, Ledger WJ. Clinical Management of
Vulvodynia. Rev Gynecol Pract . 2002;2:83-90.
Physical Therapy:
Vulvar Vestibulitis Subtype
Physical therapy reduces muscle tension and spasm, decreasing pain levels by 40-60%
*
Physical therapist can retrain dysfunctional pelvic floor muscles
* Hartmann EH, Nelson C. The Perceived Effectiveness of Physical Therapy Treatment on Women
Complaining of Vulvar Pain and Diagnosed With
Either Vulvar Vestibulitis Syndrome or Dysesthetic
Vulvodynia. Journal of the Section on Women’s
Health . 2001;25:13-18.
Physical Therapy:
Vulvar Vestibulitis Subtype
Physical therapy components:
Pelvic floor exercise
Myofascial release
Trigger point pressure
Massage
Resource: The American Physical Therapy
Association (800-999-APTA) or
(www.apta.org)
Medical Management:
Vulvar Vestibulitis Subtype
Topical estrogens:
Improve epithelial maturation
Inhibit production of inflammatory mediators
(cytokines and interleukin-1)
Lower pain threshold
*
*Cutolo M,Sulli A,Seriolo B,et al.Estrogens,the immune response and autoimmunity.Clin Exp
Rheumatol.1995;13:217-226
Medical Management:
Vulvar Vestibulitis Subtype
Topical estrogen creams useful for women with thin vaginal epithelium and/or lose of vulvar adipose tissue
Can be used with other pharmacologic agents
Medical Management:
Vulvar Vestibulitis Subtype
Tricyclic antidepressants
(Amitriptyline-10mg hs: dose up to 150mg daily)
Fluconazole
Gabapentin (anticonvulsant),
Venlafaxine-efficacy not proven
Selective serotonin receptor inhibitors (SSRIs)-efficacy not proven
Medical Management:
Vulvar Vestibulitis Subtype
Corticosteroids: (topical and injections)
Topical anesthetics
(nitroglycerin & lidocaine)
Alpha Interferon injections
Capsaicin cream (immune response modifier)
Surgical Management:
Vulvar Vestibulitis Subtype
Excision of affected vulvar area to remove neural hyperplasia
Surgery reserved for nonresponders to conservative treatments
Data suggest a success rate varying from 40-100%
Long term data lacking
Surgical Procedures:
Vulvar Vestibulitis Subtype
Types: focal excision, vestibuloplasty, vestibulectomy and perineoplasty
Vestibulectomy excises a U shaped area of the vestibule from 5mm lateral to the urethra and the posterior fourchette
Perineoplasty excises the vestibule from below and lateral the urethral meatus to the anal canal with the vaginal mucosa undermined 1-2cm.
Pharmacologic Management:
Dysesthetic Vulvodynia Subtype
Amitriptyline: first line therapy
Other tricyclic antidepressantsdesipramine and imipraminemay be effective
*
Selective serotonin reuptake inhibitors efficacy not proven
* McKay M. Dysesthetic Vulvodynia: treatmnet with amitryptyline. J Reprod Med 1993 ; 38:9-13