Vulvar Vestibulitis What is it? Vestibulitis is a chronic and persistent
advertisement

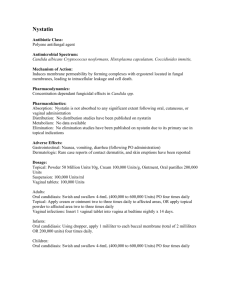
Vulvar Vestibulitis What is it? Vestibulitis is a chronic and persistent clinical syndrome characterized by pain and inflammation of the vulvar vestibule. The vestibule itself is comprised of the inner aspect of the labia up to the hymenal ring, which is the entry point to the vagina. What are the symptoms? Women typically complain of a burning sensation in that region or discomfort on penetration during intercourse. What causes it? The cause of vulvar vestibulitis is unknown. Researchers have proposed that that inflammation may be caused by infections (bacterial, viral, or fungal), contact dermatitis, allergic response, hormonal changes, or it may be a disorder of the muscles of the pelvic floor. The persistent pain of vulvodynia is thought to result from dysregulation of the pelvic nerves similar to that experienced by people who have pain following an outbreak of shingles (herpes zoster infection), long after the lesions from the infection have cleared. How is it diagnosed? Three criteria are used to diagnose vestibulitis; these are known as Friedrich's criteria. They include 1. Severe pain upon touching the vestibule or upon attempted vaginal entry, 2. Tenderness localized within the vestibule (usually a gynecologist will assess this by gently touching a Qtip to the region), and 3. Redness and inflammation of varying degrees. How can it be treated? At the moment, there is no cure, so treatment is directed at symptom control. The following hygienic measures may be useful: Avoid the use of irritants including bubble bath and feminine hygiene spray. Use mild laundry soap rather than detergent. Do not use soap or when bathing or showering. Wear cotton underclothing. Use tampons instead of pads. Avoid pantyhose. Enjoy baths with warm water and sea salt (one half to one cup of sea salt). Apply an ice pack or bag of frozen peas to help ameliorate the burning sensation which can accompany this condition. Soothing lotions may offer some relief. Consider trying simple, non-perfumed lubricants, such as Vaseline Replens Barrier creams Gold Bond Udderly Smooth Hydrocortisone 0.5% Topical anesthetics can also be useful. They include: Maintain Xylocaine 5% ointment Massage the gel into the skin of the tender areas, then soak a cotton ball in the gel and leave it in the vestibule overnight. A recent trial published in Obstetrics and Gynecology in 2003 shows some evidence that 5% xylocaine ointment used nightly in this manner for six to seven weeks provided some relief of symptoms in 76% of the women enrolled in the trial. A topical anesthetic may be used prior to intercourse. Women who continue to have intercourse have the best chance of eventual cure of their vestibulitis. Non-genital stimulation and pleasuring are encouraged with vaginal penetration kept brief. A peeled cucumber or carrot may be used as a dilator if desired. No prescription medications have been found to consistently control the symptoms of vulvar vestibulitis. herapeutic trials have employed cromolyn topical ointment (an anti-inflammatory agent), topical estrogen, and capsaicin cream (directed at a pain-mediating molecule). None of these proved to be a reliable treatment for vestibulitis. Surgical treatment of vestibulitis is considered to be a last resort and may not provide relief of symptoms. Physiotherapy targeting the muscles of the pelvic floor has also shown promise, eliminating some of the muscle spasm that accompanies chronic vulvodynia. Kegel's exercises (contracting and releasing the pelvic floor muscles) may be useful to gain conscious control over vaginal muscle spasms. At this point, no one therapy has been shown to completely eliminate the distressing symptoms experienced by women suffering from vulvar vestibulitis. The hygienic measures and treatments outlined above, however, may keep these symptoms under control, and help women live more comfortably with this syndrome.