Redondo Beach, CA
May 20, 2013
Vickie
Jenni Gabelsberg DPT, MSc, MTC, WCS, BCIA-PMDB
Owner/Director Women’s Advantage, Inc.
Torrance, CA
Subjective Summary
History
of hysterectomy and bladder sling
with mesh 4 years prior
History
of mild urinary frequency and
nocturia 2x/night
4
months before eval, self treated a yeast
infection with Monistat
Subjective Summary
At
eval: pt could not sit or walk prolonged,
wear tight clothing/jeans, or tolerate
intercourse
Urethral
pressure with sitting
Severe
pain at vestibule, worsened by touch,
and worst at night
Pain
rated as 10/10 without neurontin and
3/10 with meds (300 mg TID)
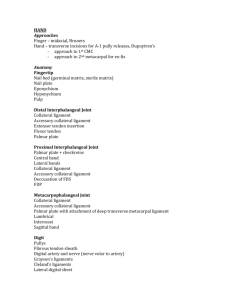
Objective Findings
Red
irritated vestibule at 4 and 8 o’clock
positions, mild tenderness with Q Tip test
Thinning
PFM
and pale labia
MMT 2/5 (poor) with a 2-3 second hold
Objective Findings
Hypertonus and pain found with palpation of:
Bulbocavernosus, ischiocavernosus, STP
(severe)
Urogenital
diaphragm ms (mild)
Pubococcygeus,
OI (moderate)
iliococcygeus, coccygeus and
Objective Findings
Tightness
found in bilateral hamstrings,
adductors, iliopsoas, piriformis and gluteal
muscles (with poor connective tissue
mobility)
Weak
abdominal, lumbar and pelvic girdle
stabilizers
Beginning Physical Therapy Treatments:
Intravaginal
LE
Manual Therapy
and trunk stretching
Biofeedback
evaluation – modified Glazers
protocol given for HEP
Cold
laser
Beginning Physical Therapy Treatments:
Connective
Tissue Mobilization:
Adductors
Anterior thigh and inguinal region
Labia
Abdomen
Posterior thigh
Gluteals
Piriformis
Obturator
Internus
Cold Laser Treatments:
Also known as low level light therapy, NON thermal
Effects:
Increase ATP at cellular level
Stimulation of mitochondria, cellular enzymes,
macrophage activation, collagen synthesis, increase
in granulation tissue, increased serotonin and
endorphin with decreased c fiber (pain) activity.
Uses: inflammatory conditions, wound care and tissue
repair, pain control
Progress Assessment – Two Months:
30-40% improvement in vulvar pain
Able to sit 20-40 minutes depending on the surface
Still unable to wear tight clothing
Decreased external vestibular pain by 95%
Able to tolerate orgasm but pain/”tingling”
continued for 24 hours after
Zero penetration
Progress Assessment – Three Months:
Zero pain at vestibule with touch
Brief shooting pains at anterior vulva
Tingling nerve pain remains 80% of the time, worsens with
sitting
Can put on jeans and zip up, but has not tried sitting or
wearing out
Still wearing sweat pants all the time
30-40 min sitting tolerance – better on soft surfaces
Describes feelings of pelvic “congestion” and “heaviness”
Treatment additions:
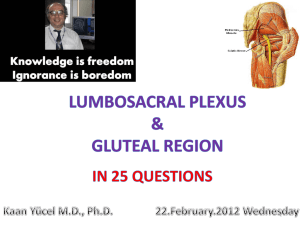
Began
neural glides of the pudendal nerve
Added
sacrotuberous ligament release
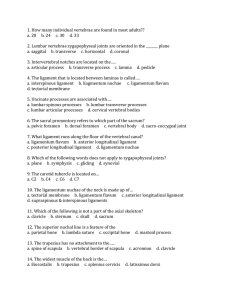
It will cross under the
piriformis, leaves the
pelvis through greater
sciatic foramen, then
back through lesser
sciatic foramen, over
the sacrospinous
ligament, under the
sacrotuberous
ligament
Dorsal nerve of the
clitoris or penis
2. The perineal branch
Urethral sphincter
Perineal muscles
and sensation
3. The inferior rectal or
hemorrhoid nerve
External anal
sphincter (EAS)
Perianal sensation
1.
Obturator
Internus
Sacrotuberous
Ligament
Sacrospinous
Ligament
Progress Assessment – Six to Seven Months:
75%
overall improvement, pain rated 4-5/10
Now
able to wear jeans 5-6 hours, able to wear
underwear
Able
to sit through dinner with her family
Able
to sit on a hard surface 5-10 minutes, soft
surface for 2 hours
Able
to have intercourse with no vulvar or
vaginal pain during
Progress Assessment – Ten to Eleven Months:
80-85%
improvement, pain rated 2-3/10
Sitting
is still her most pain provoking activity
Now
able to walk up and down hills, stairs and
do pilates
Able
Meds
to sit 3 hours at hairdresser
– Estrace 3x/wk, Neurontin increased to
2400 mg/day
Treatment additions:
Thoracic
and lumbar joint mobilizations
Heat
and Interferential electrical stimulation to
thoracic spine
Given
a TENS unit to do EMS at home
Postural
education/core training
Progress Assessment – One Year:
90% improved
Sitting still limited by vulvar and buttock/posterior
thigh pain
Able to walk 7 miles at beach with zero exacerbation
in symptoms
External vulva healthy
Pain free standing tolerance
Able to wear jeans and underwear all day
Treatment additions:
Increased
external manual therapy to levator ani
ms, adductor attachment onto pubic rami,
Obturator Internus ms, coccygeus
Focused
and OI
internal MT to iliococcygeus, coccygeus
Recent Changes:
April
11, 2013 had first caudal nerve block with
significant improvement in nerve pain, zero
radiating buttock pain, scheduled for weekly
injections
Pt treatments focus on:
External MT to levator ani, adductors
CTM to adductors
Recent Changes:
Intravaginal
MT to urogenital diaphragm and
levator ani ms
ART to proximal hamstrings
Hip mobilizations with neuromuscular re-ed, glut
strengthening
Heat with IFC/EMS to gluteals and lumbosacral
spine
Neural Glides to Pudendal nerve
Cold laser
Current Status
90%
improved
Pain
continues to “move around pelvis”
Most
consistent pain is buttock pain with any
prolonged sitting
Able
to participate in family activities, camping,
exercise