common-symptoms-handsout
Common benign gynecological disorders
Vulvar pain
Professor Jacob Bornstein
Western Galilee Hospital, Nahariya, Israel
Test for Vestibulitis
Vulvar Vestibulitis:
Friedrich’s criteria of diagnosis
1. Severe pain with vestibular touch
2. Sensitivity is limited to the vestibule
3. Erythema of various degrees (may be absent)
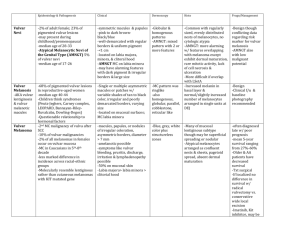
Outcome of surgery for Vulvar Vestibulitis
Age
17-80
Follow-up in years
CR
0.2-10
PR
371
(57%)
103
(16%)
Outcome
NR CR+
PR
104
(16%)
68
(11%)
Total
646
(100%)
Bornstein et al. Obstet Gynecol 1999;93:876-880
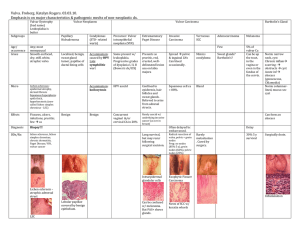
Vulvar pruritus
• Lichen Sclerosus
• How to do a vulvar biopsy
• Approach to chronic vulvar pruritus
Clinical characteristics of
Lichen Sclerosus:
1. Lichenification and vulvar + perianal pruritus
5. Lichenification, including thickening of the skin, a thick keratin layer and emphasizing the skin fissures
6. Fissure
2. Second stage – Thinning of the labia minora mucosa, rendering it easy to become lacerated
7. Involvement of the vulvar and perianal area in the figure of “8”
3. The anterior parts of the labia minora adhere to each other and produce Phymosis covering the clitoris
4. Ecchimoses – sign of scrathing the skin
8. Stenosis of introitus –
“Kraurosis”
9. Rare prior to adolescence.
Spontaneously resolve after puberty in 50%
10. Rarely extra-genital –
Forearm and breasts
Keye’s dermal punch
Vulvar biopsy
Principles of taking a vulvar biopsy
•Sterilization
•Topical anesthetic – Esracaine,
Emla
•Local anesthetic
•Sample the ulcer’s margin
•Take several biopsies from a large lesion
•Do not compress the specimen
•Immerse in Formalin immediately
Side effects of local anesthetic - Lidocaine
•Dizziness
•Tinnitus
•Peri-oral itch
•Metal taste
•Tremor
•Convulsions
•Myocardial depression
Lichen Sclerosus
Histopathologic diagnostic criteria:
1. Thin hyperkeratotic layer
2. Thinning of the epithelial layer
3. Flatenning of the papillae
(Rete pegs)
4. Homogenization of the stroma
5. Deep lymphocitic infiltration
Lichen Sclerosus histopathologic diagnostic criteria (Repeat):
1. Thin hyperkeratotic layer
2. Thinning of the epithelial layer
3. Flatenning of the papillae (Rete pegs)
4. Homogenization of the stroma
5. Deep lymphocytic infiltration
Lichen Sclerosus: Etiology
• chronic inflammation / atrophy
• autoimmune disease
• deficiency in dehydro-Testosterone
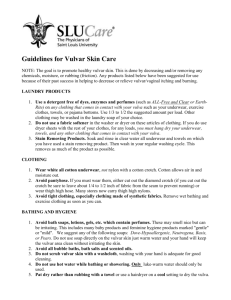
Treatments for Lichen sclerosus
Local steroids Genital care
Symptomatic treatment
Clobetasol propionate 0.05%
Sitz baths avoid strong soaps -
Anti-histamine (Otarex)
Emla 5%; Eurax 10%
-Avoid tight synthetic underwear
Dermovate (Clobetasol
Propionate 0.05%)
Cream or Ointment
Instruction for the use of Dermovate:
•Twice a day for two weeks
•Once a day for one month
•Twice a week for two months
•As needed
Follow up
• 3 month assesment
• 6 month follow-up
• 1 yearly follow-up
• Every persistent ulceration or new growth must be examined – risk of malignant transformation: 3%-5%