Management of Urinary Tract Infections
advertisement
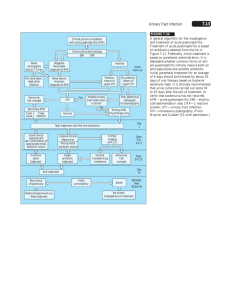
Management of Urinary Tract Infections Definitions: Uncomplicated cystitis: Limited to the lower urinary tract and occurs in older children (older than two years) or adolescents with no underlying medical problems or anatomic or physiologic abnormalities. Most often it is caused by pathogens susceptible to the antimicrobial agents usually used to treat cystitis. Patients present with dysuria, frequency, urgency, suprapubic pain and/or hematuria. Complicated cystitis: Associated with upper tract disease (pyelonephritis), multiple-resistant uropathogens, or hosts with special considerations such as immunocompromised patients or anatomic or physiologic abnormalities, or an indwelling bladder catheter. Patients who have urodynamic dysfunction, neurogenic bladder, or incomplete bladder emptying may harbor pathogens in residual urine, thereby creating a source for persistent or recurrent infection. Uncomplicated pyelonephritis: Upper urinary tract infection that presents with fever (>38ºC) (though may be absent early on), chills, flank pain, costovertebral angle tenderness, and nausea/vomiting, +/- signs or symptoms of acute cystitis. Pathogens are often more resistant to typical antibiotics than those leading to cystitis. Complicated pyelonephritis: Progression of upper urinary tract infection to emphysematous pyelonephritis, renal corticomedullary abscess, perinephric abscess, or papillary necrosis. **Although children with pyelonephritis tend to present with fever, it is often difficult on clinical grounds to distinguish cystitis from pyelonephritis, particularly in young children (those younger than two years). Microbiology: Escherichia coli is the most common bacterial cause of UTI; it accounts for approximately 85 percent of UTI in children and adolescents. Other gram-negative bacterial pathogens include Klebsiella, Proteus, Enterobacter, and Citrobacter. Gram-positive bacterial pathogens include Staphylococcus saprophyticus, Enterococcus, and, rarely, Staphylococcus aureus. *** See attached Antibiogram for local sensitivities 2011 AAP Infant and Child Management Recommendations: Diagnosis: To establish diagnosis of UTI in infants less than 2 years of age one should require both urinalysis suggestive of infection (pyuria and/or bacteriuria) AND at least 50,000 CFUs/mL of a uropathogen from a catheterization or a SPA. Treatment: Standard empiric therapy for urinary tract infection in children less than 2 years of age is a 3rd generation cephalosporin. Amoxicillin and ampicillin are not routinely recommended for empiric therapy because of the high rate of resistance of E. coli. Similarly, amoxicillinclavulanate, 1st generation cephalosporins (eg cephalexin), and TMP-SMX should be used with caution because of the increasing rates of resistance to these drugs. Use of Fluoroquinolones: They are effective for E. coli, and resistance is much less common. However, the safety of quinolones in children is still under study. Currently they remain a potential first-line agent only in the setting of pyelonephritis or complicated UTI when typically recommended agents are not appropriate on the basis of susceptibility data, allergy, or adverseevent history. The 2006 and 2011 AAP policy statement supports the use of ciprofloxacin as oral therapy for UTI and pyelonephritis caused by P. aeruginosa or other multidrug-resistant Gramnegative bacteria in children aged 1 through 17 years. Agents that are excreted in the urine but do not achieve therapeutic concentrations in the bloodstream, such as nitrofurantoin, should not be used to treat febrile infants with UTIs, because parenchymal and serum antimicrobial concentrations may be insufficient to treat pyelonephritis or urosepsis. **If patient has had previous urinary tract infections in the past always investigate the prior uropathogen’s sensitivities to help guide treatment. Indications for hospitalization and/or parenteral therapy include: Age <2 months Clinical urosepsis (eg, toxic appearance, hypotension, poor capillary refill) Immunocompromised patient Vomiting or inability to tolerate oral medication Lack of adequate outpatient follow-up (eg, no telephone, live far from hospital, etc) Failure to respond to outpatient therapy Complicated pyelonephritis Acceptable inpatient treatment regimens include the combination of ampicillin and gentamicin gentamicin alone; or a third- or fourth-generation cephalosporin. Ampicillin should be included if enterococcal UTI is suspected. Length of treatment: First episode of uncomplicated cystitis in older children (older than two years) who are afebrile be treated for five to seven days. Complicated UTI (including all those less than 2 years) should undergo treatment for 10 days with a range of 7 to 14 days. Follow Up Imaging: Febrile infants with urinary tracts infections should undergo renal/bladder ultrasonography once infection has resolved. VCUG is no longer recommened routinely after first febrile UTI. VCUG is ONLY indicated if the renal ultrasound shows ydronephrosis, scarring, or other findings suggestive of high grade VUR or obstructive uropathy, recurrence of febrile UTI, or other atypical or complex clinical circumstances. Adolescent Caveats: Nitrofurantoin can be considered as a potential first line treatment for a post-pubertal adolescent with uncomplicated cystitis. Most cases of uncomplicated pyelonephritis can be managed as an outpatient. However, patients who appear ill, or have significant pain may have severe pyelonephritis or a complication of acute pyelonephritis and should be considered for hospitalization and further evaluation. References: Bradley JS, Jackson MA, Committee on Infectious Diseases, American Academy of Pediatrics. The use of systemic and topical fluoroquinolones. Pediatrics 2011; 128:e1034. Colgan, R. Williams, M. Johnson, J. Diagnosis and Treatment of Acute Pyelonephritis in Women. Am Fam Physician. 2011;84(5):519-526. Colgan, R. Williams, M. Diagnosis and Treatment of Acute Cystitis in Women. Am Fam Physician. 2011;84(7):771-776. Montini G, Tullus K, Hewitt I. Febrile Urinary Tract Infections in Children. N Engl J Med 2011; 365:239-250. Subcommittee on urinary tract infection, steering committee on quality improvement and management. Urinary Tract Infection: Clinical Practice Guideline for the Diagnosis and Management of the Initial UTI in Febrile Infants and Children 2 to 24 Months. Pediatrics. 2011;128(3): 595-610.