Review_Table_URI__PN
advertisement

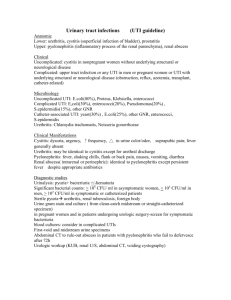
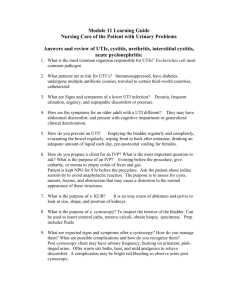
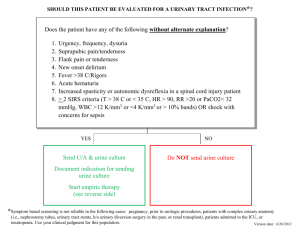
UTI and Pylonephritis (PN): Sarah Eisenschenk URI PN Terminology/defin itions Organisms Microbial colonization of urine and tissue invasion of any structure of the urinary tract is broadly called UTI. Clinically, UTI usually refers to involvement of lower tract structures while pyelonephritis refers to involvement of upper tract structures Bacteria: E. coli > 90% cases. Proteus (produces urease, NH3+), Klebsiella, Staph saprophyticus, Pseudomonas, Enterobacter, Enterococci Yeast Candida, especially in diabetics or OTHER (IC) patients Fungi – IC patients Viruses Body’s Defense Mechanis m Urine: the following inhibit bacterial replicatio n: Acid pH, ↑ urea, ↑ osmolality Dynamics of urinary flow – wash out Risk Factors Clinical Presentation Laboratory Evaluation Females >>> males due to short urethra which results in easier ascension and migration of perineal/large bowel bacteria to bladder where infection may occur. ↑ urinary frequency, Dysuria, Suprapubic discomfort/pressure, Cloudy & malodorous urine, Fever: not as common, but can occur (even rigors), Flank pain: not often, but can occur, Hematuria: usually not gross CBC: usually see leukocytosis. Much more likely to see significant ↑ of WBC in pyelonephritis *Clinical pearl: Beware elderly patients and immunocompromised patients who may not mount this response Urinalysis - How to obtain: 1. Clean-catch midstream sample 2. Catheterization 3. Suprapubic aspirate (mostly infants) 4. Laboratory Evaluation (cont’d) Urinalysis – Positive findings for UTI and pyelonephritis include: Nitrites: surrogate marker for bacteriuria; Leukocyte esterase: reflects presence of WBCs; Proteinuria: more commonly in pyelonephritis; Pyuria: > 10 WBC/hpf on centrifuged specimen: important number; Hematuria: few RBCs to gross hematuria depending on body’s response, degree of tissue invasion/inflammation and organism; Bacteriuria on light microscopy with or without Gram staining Culture: Helps to define organism, antibiotic sensitivity - Should be done routinely on all men, children, and patients with risk factors in addition to female status - If first episode for a female, culture not required but if patient has history of recurrent infections or is pregnant or has immunosuppression, including diabetes, culture should be done - Positive culture usually defined as ≥ 10,000 cfu of bacteria per ml of urine obtained on clean-catch midstream specimen - Catheterized or suprapubic specimen may be considered positive if > 100 cfu are found due to fewer contaminants - Radiology: Ultrasound, CT, IVP, MRI; usually done if patient not responding to treatment in 2-3 days Instrumentation: cystoscopy, catheterization (short-term and long-term) Structural or anatomical anomalies of GU tract, i.e., posterior urethral valves, medullary sponge kidney, polycystic kidney, benign prostatic hyperplasia (BPH), stones, cystocele, etc. Functional anomalies: Vesicoureteral reflux (often seen in children) & Neurogenic bladder Intercourse: “Honeymoon cystitis”; void immediately after intercourse Pregnancy = ↑ incidence of bacteriuria Age: Elderly = ↑ rates of bacteriuria Up to 40% of elderly patients - Usually patient has many similar symptoms as UTI but often significant fever (38.9 to 40º C.) - Often see nausea, vomiting - Commonly CVAT, flank pain - Abdominal pain (upper/lower), altered GI function (diarrhea, ileus) and fatigue may be seen *Clinical Pearl* UTI, pyelonephritis, and urethritis share many similar symptoms. The more toxically ill the patient appears, the more likely it is that he/she has pyelonephritis. UTI and Pylonephritis (PN): Sarah Eisenschenk Treatment: Antibiotics - po vs. parenteral Empiric: TMP/SMX is still first-line therapy (E. coli resistance may be up to 20% in some areas) Quinolones (≥18 yrs) Nitrofurontoin (resistance rates generally low for E. coli) Cephalosporins Amoxicillin (not used very often) When To Refer (to Urology, Nephrology, Infectious Disease) Renal papillary necrosis diabetics with significant vascular disease and severe pyelonephritis analgesic abusers patients with rapidly decompensating course due to ischemic necrosis of papilla and medulla diagnosis made by pyelogram and/or urinary sediment examination for papillary tissue Antifungals (in immunocompromised.) Symptomatic: Pyridium (In will cause urine to turn orange and will stain contact lenses.) Often occurs as extension of pyelonephritis process Fluids po or IV important: Remember dynamic urinary flow washout principle. Water and juice are best. Consider staph spread hematogenously from a distant source (endocarditis) Prophylaxis: indicated for patients with recurrent infections (defined as 3 or more UTIs documented by urine culture within one year). Imaging studies such as CT, US, and IVP helpful Surgical drainage usually needed Treatment strategies are as follows: Acute self-treatment with 3-day course of standard therapy Post-coital dosing with TMP/SMX Continuous daily prophylaxis with low dose nitrofurantin, trimethoprim, or TMP/SMX for 6 months Renal abscess When To Refer (cont’d) Perinephric abscess Often difficult to diagnose Most patients have diabetes mellitus or stone disease and have had recent UTI Uncomplicated UTI with no previous history = may treat with 3 days antibiotics Patients present with fever and unilateral flank pain UTI in pregnancy: 7 days recommended Usually the perinephric abscess occurs secondary to the rupture of an intrarenal abscess UTI in complicated cases (i.e., sx > 1 week, diabetic, immunosuppressed): 7 days recommended Surgical drainage is needed Nephrolithiasis with infection Treatment- Pylonephritis Staghorn calculus or struvite calculus is formed by a rapidly growing stone which tends to fill the pelvocalyceal system. Stones are composed of magnesium ammonium phosphate (struvite) which represents a common sequela of urinary tract infections Proteus mirabilis is the most common organism associated with urolithiasis, but organisms such as Pseudomonas aeruginosa, Klebsiella species, Escherichia coli, and Staphylococcus aureus are also known to promote stone formation May have obstruction of ureter with high grade hydronephrosis Surgical intervention may be necessary Uncomplicated, outpatient: 7 days of Cipro has higher success rate than 14 days TMP/SMX (JAMA 283:1583, 2000) He treats with 10 days and has close follow-up to ensure their symptoms are improving. Hospitalized: IV Abx - FQ usually, but Amp/Gent and AM/SB are alternatives. Treat until afebrile 24-48º, then switch to po and treat for total of 2 weeks Complicated pyelo: usually cath-related Treat for 2-3 weeks total with combination IV and po Abx Atypical organisms, usually in immunocompromised patients Candida Fungi