RPO UTI Memo
advertisement
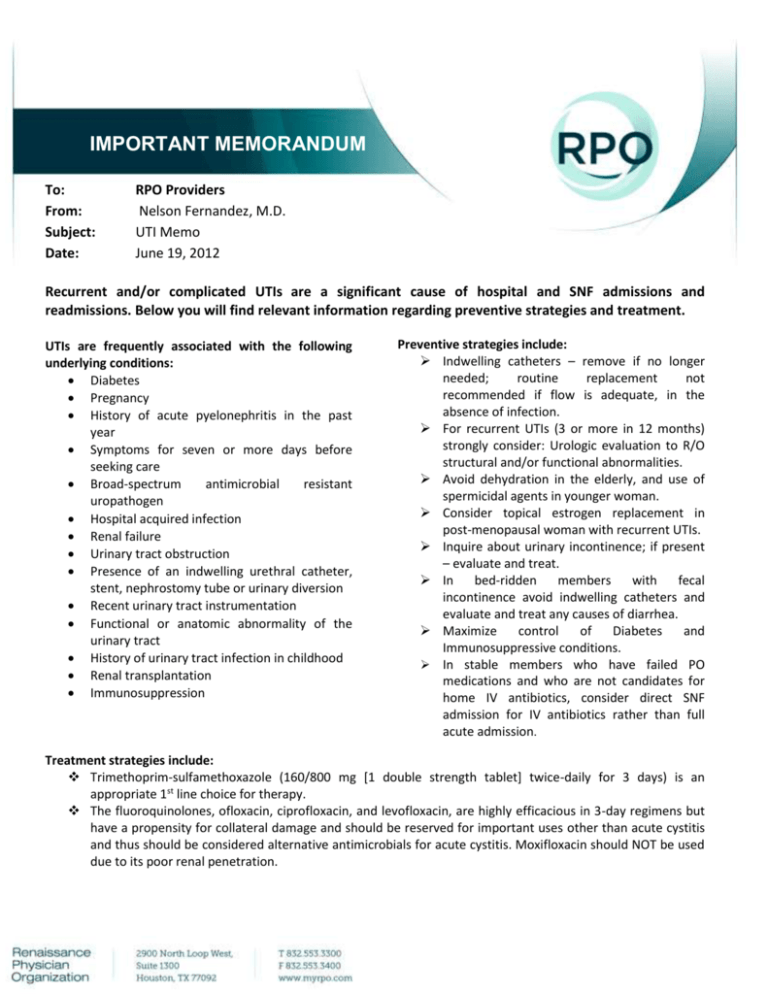
IMPORTANT MEMORANDUM To: From: Subject: Date: RPO Providers Nelson Fernandez, M.D. UTI Memo June 19, 2012 Recurrent and/or complicated UTIs are a significant cause of hospital and SNF admissions and readmissions. Below you will find relevant information regarding preventive strategies and treatment. UTIs are frequently associated with the following underlying conditions: Diabetes Pregnancy History of acute pyelonephritis in the past year Symptoms for seven or more days before seeking care Broad-spectrum antimicrobial resistant uropathogen Hospital acquired infection Renal failure Urinary tract obstruction Presence of an indwelling urethral catheter, stent, nephrostomy tube or urinary diversion Recent urinary tract instrumentation Functional or anatomic abnormality of the urinary tract History of urinary tract infection in childhood Renal transplantation Immunosuppression Preventive strategies include: Indwelling catheters – remove if no longer needed; routine replacement not recommended if flow is adequate, in the absence of infection. For recurrent UTIs (3 or more in 12 months) strongly consider: Urologic evaluation to R/O structural and/or functional abnormalities. Avoid dehydration in the elderly, and use of spermicidal agents in younger woman. Consider topical estrogen replacement in post-menopausal woman with recurrent UTIs. Inquire about urinary incontinence; if present – evaluate and treat. In bed-ridden members with fecal incontinence avoid indwelling catheters and evaluate and treat any causes of diarrhea. Maximize control of Diabetes and Immunosuppressive conditions. In stable members who have failed PO medications and who are not candidates for home IV antibiotics, consider direct SNF admission for IV antibiotics rather than full acute admission. Treatment strategies include: Trimethoprim-sulfamethoxazole (160/800 mg [1 double strength tablet] twice-daily for 3 days) is an appropriate 1st line choice for therapy. The fluoroquinolones, ofloxacin, ciprofloxacin, and levofloxacin, are highly efficacious in 3-day regimens but have a propensity for collateral damage and should be reserved for important uses other than acute cystitis and thus should be considered alternative antimicrobials for acute cystitis. Moxifloxacin should NOT be used due to its poor renal penetration. Beta-Lactam agents, including amoxicillin-clavulanate, cefdinir, cefaclor, and cefpodoxime-proxetil, in 3–7day regimens are appropriate choices for therapy when other recommended agents cannot be used. Other beta-lactams, such as cephalexin, are less well studied but may also be appropriate in certain settings. Ampicillin and amoxicillin should NOT be used due to its poor efficacy. Nitrofurantoin while considered an appropriate 1st line choice, is considered a High Risk Medication (HRM) therefore should be used only when two or more options have been used or a contraindication to other agents (i.e. allergy). If alternative medication is not appropriate please call 1-800-331-6293 for override considerations. Systemic antimicrobial prophylaxis should not be routinely used in patients with short-term or long-term catheterization, including patients who undergo surgical procedures, to reduce catheter associated (CA) bacteriuria or CA-UTI because of concern about selection of antimicrobial resistance. Important to follow up after culture and sensitivity information is available for appropriate antibiotic therapy. Prompt follow up and monitoring is recommended in complex members with multiple risk factors. If response is inadequate, please consider outpatient IV antibiotics either at patient’s home or skilled nursing facility.