Urinary Tract Infections in the Pediatric Population
advertisement

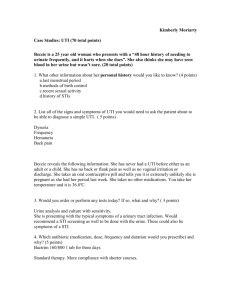
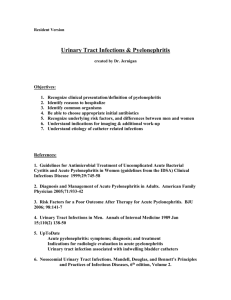
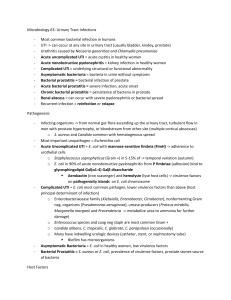
Urinary Tract Infection in the pediatric patient Meaghan Eddy, RN, BSN FNP student Definition • Includes bacterial infection of any structure within the urinary tract • A majority of UTI’s are located in the bladder or urethra • The higher up the Urinary tract, the more serious Severe and recurrent infections may lead to: • • • • Renal scarring Hypertension End-Stage Renal Dysfunction in adulthood May be life threatening in the neonate/infant Common Pathogens • E. Coli- the most common cause of uncomplicated UTI. Estimates range from 7595% on infections • Staphylococcus saprophyticus- generally more aggressive, more likely to evolve to a pyelonephritis or result in recurrent UTIs. • Entereobacteriaceae such as proteus and klebsiella less common • Group B strep- more in neonates History/ROS • Previous UTI’s? • Hygiene habits? • Voiding/Bowel habits? (frequency, dribbling, weak urinary stream, daytime enuresis) • Sexual activity, sexual abuse • Family history of VUR, recurrent UTI, kidney problems? • Presence of diaper rash, pinworms? Physiologic predisposition Uti should be a top differential in children with known: • Known vesicoureteral reflux • Congenital malformations of urinary tract structures • Disturbances in neurologic function such as a myelomeningeoceal, hydrocephalus, cerebral palsy Risk Factors in General Population • Caucasians (2-4x higher than AA) • Females (2-4x higher than circumcised males) • Preterm and Low Birth-weight infants • Uncircumcised males during first year of life • Bottle-fed infants (lack of IgA provided in breastfeeding to fight mucosal invasion by bacteria) Risk Factors Cont’d • Familial Predisposition • Sexual Activity, specifically use of spermicidal condoms/foams • Dysfunctional Voiding cause in 40% of toilet trained children with first UTI, 80% in those with recurrent UTI Clinical Findings (by age group) Neonates • • • • • • • • Jaundice Hypothermia FTT Sepsis Vomiting/Diarrhea Cyanosis Abdominal Distension Lethargy Infants • • • • • • • • Malaise Irritability Difficulty Feeding FTT Fever (esp. in pyelonephritis) Vomiting/Diarrhea Malodorous Urine Abdominal Pain/colic Toddlers/Preschoolers • • • • • • • Changes to voiding pattern Malodorous urine Abdominal/Flank pain (esp. in pyelonephritis) Enuresis Vomiting/diarrhea (esp. in pyelonephritis) Fever Diaper rash if not potty trained School-Age to Adolescence • • • • • • • Frequency, Urgency, Discomfort Malodorous Urine Abdominal/Flank Pain (esp in pyelonephritis) Suprapubic tenderness Fever/Chills (esp. in pyelonephritis) Malaise Vomiting/diarrhea (esp. in pyelonephritis) Other physical exam findings • Females may have vaginal erythema, edema, irritation, or discharge; presence of labial adhesions • Parents may report a weak, dribbling stream with urination • Presence of sacral dimpling, decrease in perineal sensation, decrease in lower extremity reflexes Diagnostic studies Urine Specimen not all collection methods are created equal! Suprapubic bladder aspiration -99% accurate -should consider in very ill children Clean catch -catch midstream void -first morning’s urine -refrigerate until culture -have female sit backward on toilet to separate labia and decrease contamination Bag collection -high degree of contaminants -only useful to rule out UTI Straight cath -95% sensitivity -should be used in very ill children and infants Pertinent findings on UA **UA is not diagnostic** • Cloudiness suspicious • Leukocyte esterase: detects pyuria • Nitrites- will only be present in urine sitting in bladder >4 hours, with gram-negative bacteria • presence of more than five white blood cells • bacteria viewed per high-powered microscope field of the spun urinary sediment ?? Differential Diagnosis ?? • Infants: bacteremia, meningitis • Children: Vulvovaginitis, STI, Vaginal foreign body, Sexual Abuse, Abdominal Disease, Renal Calculi, dysfunctional voiding, dysuria-pyuria syndrome, appendicitis, pelvic abscess, pelvic inflammatory disease Urine Culture/Sensitivity *Diagnostic of UTI* Always order in presence of suspicious symptoms, even if UA is normal Positive organism ID and sensitivity Culture results of more than 100,000 cfu/ml, 50,000 in children 2-24mo per AAP guidelines Repeat culture if growth is around 10,000 cfu/ml unless collected by aspiration/catheterization- then diagnostic Additional Labs to think about: • • • • • CBC ESR C-reactive Protein BUN/Cr Blood Cultures If the child appears ill, is less than 12 months, or pyelonephritis is suspected Recommendations for anti-microbial therapy Inpatient treatment Intravenous options: • • • • • • • • Ceftriaxone 75 mg/kg every 24 h Cefotaxime 150 mg/kg/d divided every 6 h Ceftazidime 150 mg/kg/d divided every 6 h Cefazolin 50 mg/kg/d divided every 8 h Gentamicin 7.5 mg/kg/d divided every 8 h Tobramycin 5 mg/kg/d divided every 8 h Ticarcillin 300 mg/kg/d divided every 6 h Ampicillin 100 mg/kg/d divided every 6 h Oral Antibiotic options • Amoxicillin 20–40 mg/kg/d in 3 doses • Sulfonamides: -TMP in combination with SMX (6–12 mg TMP, 30–60 mg SMX per kg per d in 2 doses) -Sulfisoxazole 120–150 mg/kg/d in 4 doses • Cephalosporins: -Cefixime 8 mg/kg/d in 2 doses -Cefpodixime 10 mg/kg/d in 2 doses -Cefprozil 30 mg/kg/d in 2 doses -Cephalexin 50–100 mg/kg/d in 4 doses -Loracarbef 15–30 mg/kg/d in 2 doses 10-14 day Courses with Best cure rates per AAP Patient/Parent Education (for the uncomplicated patient) • Avoid bubble baths • Avoid Tight fitting clothing (girls) • Wipe “back to front” • Don’t hold urine for long periods of time So, a UTI is diagnosed, antibiotics are started…. but When is further testing needed? • New AAP guidelines released August 2011 • Children ages 2-24 months included in the new guidelines Options for further testing include: Renal/bladder ultrasound Voiding cystourethrography (VCUG) Intravenous pyelogram (IVP) DSMA scan Children 2-24 months • Ultrasound should be performed of kidneys/bladder for detection of anatomic abnormalities in all pts. • Perform U/S promptly if no improvement of symptoms after 48 hours of antibiotics • VCUG no longer recommended after febrile UTI unless ultrasound is abnormal or this is a recurrent problem • No recommendations for prophylactic antibiotics in children with no VUR, or VUR grades I-IV. Children older than 24 months • Recommendations vary greatly • Most recommend ultrasound at minimum for any child with pyelonephritis, suspicious factors such as HTN, weak urine stream, family history of UTI, known abnormal voiding patterns • VCUG recommended in children less than 5, with abnormal ultrasound, presence of abnormal voiding before uti • Consider VCUG in a febrile or highly complicated UTI **VCUG should be done 4-6 weeks after infection is cleared** Degrees of Vesicoureteral reflux What Next? • Consider DMSA scan to determine renal scarring in the presence of VUR • Grades i-iv may spontaneously resolve, less likely in older children • prophylactic antibiotics are recommended by Dept of Ped. Urology at Johns Hopkins, not recommended by AAP for 2-24mo children. recommendation is Bactrim/Septra • Consider referral to Pediatric Urology Prophylaxis options TMP in combination with SMX 2 mg of TMP, 10 mg of SMX per kg as single bedtime dose or 5 mg of TMP, 25 mg of SMX per kg twice per week Nitrofurantoin 1–2 mg/kg as single daily dose Sulfisoxazole 10–20 mg/kg divided every 12 h Nalidixic acid 30 mg/kg divided every 12 h Methenamine mandelate 75 mg/kg divided every 12 h References American Academy of Pediatrics. (2011). Practice Parameter: The Diagnosis, Treatment, and Evaluation of the Initial Urinary Tract Infection in Febrile Infants and Young Children. Pediatrics, 103(4), 843-852. Burns, C.E., Dunn, A.M., Brady, M.A., Starr, N.B., & Blosser, C.G. (2009). Pediatric Primary Care (4th ed.). St. Louis, MO: Saunders Elsevier Johns Hopkins Medicine. (2012). Vesicoureteral Reflux. Retrieved from http://urology.jhu.edu/pediatric/diseases/reflux.php .