Module # 9 UTI/Pyelonephritis
advertisement

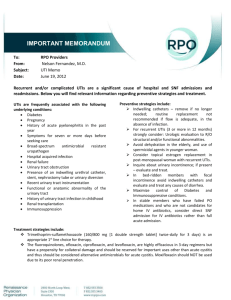
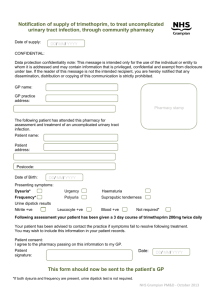
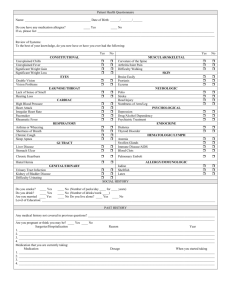
Facilitator Version Module # 9 UTI/Pyelonephritis Created by Dr. Richard Vestal May 2014 Objectives: 1. Understand the clinical features associated with a urinary tract infection and be able to develop a differential diagnosis for such symptoms 2. Understand the utility of the various features of the urinalysis and urine culture in diagnosing a urinary tract infection, and know when such tests are clinically indicated 3. Understand the comorbid conditions that distinguish uncomplicated from complicated urinary tract infections and be able to distinguish the differences in managing these conditions References: 1. Bent S et al (2002), Does this woman have an acute uncomplicated urinary tract infection? JAMA, 287(20):2701 2. Pappas, PG (1991), Laboratory in the diagnosis and management of urinary tract infections. Medical Clinics of North America, 75(2):313 3. Echols, RM (1999), Demographic, clinical and treatment parameters influencing the outcome of acute cystitis. Clinical Infectious Diseases, 29(1):113 4. Hooton, TM (2012), Clinical Practice. Uncomplicated urinary tract infection, New England Journal of Medicine, 366(11):1028-37 5. Gupta, K et al (2011), International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: A 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clinical Infectious Diseases, 52(5):e103 6. Geerlings, SE et al (2013), SWAB Guidelines for Antimicrobial Therapy of Complicated Urinary Tract Infections in Adults. Stichting Werkgroep Antibioticabeleid. Case A 27-year-old female presents to your clinic complaining of a two-day history of pain with urination that started abruptly. The patient denies any fevers or chills. She is sexually active with two male partners and uses barrier protection occasionally. She has noticed that her urine is darker in color and that she is urinating more frequently, but denies any vaginal discharge, redness or pruritus. She has had two similar episodes remotely several years ago, but did not present for evaluation due to a lack of medical insurance. Both of these episodes resolved spontaneously Vitals: Temperature - 37.3°C, Pulse - 82, Blood Pressure - 118/74, Respirations - 16, O2 - 94% ambient air On physical exam, the patient is appropriately oriented. The abdominal exam is unremarkable. The pelvic exam shows no erythema or abnormal discharge. No back pain is appreciated. What is your differential diagnosis? Acute uncomplicated cystitis should be the most likely diagnosis given the patients symptoms of dysuria and frequency. The typical symptoms of acute uncomplicated cystitis include dysuria, increased frequency, urgency, suprapubic pain and hematuria. Other diagnoses to consider include Vaginitis/Urethritis/Pelvic inflammatory disease, Interstitial cystitis a.k.a. Painful bladder syndrome and structural urethral abnormalities What additional workup would you like to perform on this patient? You can consider treating without testing at this point. The presence of one symptom of acute cystitis (see above) represents a 50% probability of a UTI. The presence of both dysuria and urgency (as is the case with our patient) is associated with a 90% probability of a UTI (in the absence of vaginitis symptoms).[1] However, many practitioners would evaluate via with urine dipstick or urinalysis. Urine dipsticks provide information about the presence of leukocyte esterase (LCE), nitrite and blood. While the presence of LCE or nitrite on a dipstick is associated with a specificity of 82%, the sensitivity of a dipstick is only 75% and is unlikely to be helpful in the evaluation of patients with a strong pre-test probability as a negative result should not affect the patient’s outcome.[1] Many providers would opt for a urinalysis at this point. Based on your history and physical exam, you decide to defer STI testing. A urinalysis is performed that shows large LCE, negative nitrite, >150 WBCs/HPF and 50 RBC/HPF and a diagnosis of acute uncomplicated cystitis is made. What significance does the presence or absence of LCE, nitrite and WBC play in the diagnosis of acute uncomplicated cystitis? LCE – The presence of LCE is highly sensitive (75-91%) for the diagnosis of a urinary tract infection, but lacks specificity (41-87%), and can represent a false positive in a number of scenarios, particularly contaminated urine samples.[2] Nitrite – The presence of nitrite is poorly sensitive (34-42%) but highly specific (94-98%) for the presence of a urinary tract infection. Nitrite would be expected to be positive in the presence of enterobacteriaceae, but may not be positive with other commonly seen organisms. [2] WBC – The presence of any WBC in the urine is highly sensitive (96%) for a urinary tract infection, and the absence of urine WBC should prompt the search for alternative diagnoses, though this can rarely be seen in the setting of unilateral pyelonephritis with obstruction. The specificity of urine WBC is poor (47%).[2] The presence of bacteria in the urine is poorly sensitive (58%) and specific (72%). [2] The above values represent any positive value. Obviously if higher thresholds are used (i.e., many bacteria vs. few), the sensitivity decreases and specificity increases. What are the most likely organisms contributing to this patient’s symptoms? The most common organisms causing a urinary tract infection are as follows:[3] Escherichia coli Proteus mirabilis Klebsiella pneumonia Other enterobacteriaceae Staphylococcus saprophyticus Uncomplicated patients growing lactobacilli, enterococci, Group B streptococci and coagulasenegative staphylococci (other than saprophyticus) most likely represent contaminated specimens.[4] What is the most appropriate therapy for this patient? (medication and duration) There are several antibiotic options for acute uncomplicated cystitis, though empiric therapy must be based on local resistance patterns (see UNM 2012 antibiogram below). Acceptable treatment options include:[5] Trimethoprim-sulfamethoxazole (One DS tablet PO BID x 3 days) -Avoid if local resistance is >20% or if the patient has taken TMP-SMX within the last 6 months Nitrofurantoin (100mg PO BID x 5 days) -Avoid if pyelonephritis is suspected -Contraindicated in CrCl < 60 Fosfomycin (3gm PO x 1 dose) Fluoroquinolone (three-day course of ciprofloxacin, levofloxacin or ofloxacin) Oral beta lactams are less effective, but can be considered. These include amoxicillinclavulanate, cefpodoxime, cefdinir and cefaclor. Each for a seven-day course. Note very high resistance rates of e.coli to TMP-SMX, amoxicillin-clavulanate and ciprofloxacin with our local antibiogram What conditions must be present to diagnose a complicated UTI and how would this affect management? 1. Genitourinary/Renal abnormalities (i.e., renal disease, urinary obstruction, genitourinary instrumentation [current or recent], functional abnormality, etc.) 2. High-risk for resistant organisms (Symptoms >7 days, hospital-acquired infection) 3. Immunosuppression (Diabetes, HIV, chronic steroid use, etc.) 4. Pregnancy These patients are at risk for a much more broad spectrum of organisms, so a urine culture is essential to help narrow the antibiotic regimen rather than completing a course of a very widespectrum antibiotic coverage. Acceptable antibiotic regimens until culture data is returned includes:[6] Amoxicillin plus an aminoglycoside (10-14 days) Second-generation cephalosporin plus an aminoglycoside (10-14 days) Intravenous third-generation cephalosporin (10-14 days) Fluoroquinolones if local resistance is <10% (ciprofloxacin 500mg po BID or 1000mg extended release PO QD; levofloxacin 750mg PO QD) for 5-14 days has a wider spectrum of coverage and achieves good urinary levels. Nitrofurantoin, TMP-SMX, fosfomycin and oral beta-lactams have poor activity against the additional organisms seen in acute complicated cystitis. The patient is started on nitrofurantoin to complete a five-day course. A follow-up nursing phone call reveals that she was compliant with her medication and has had complete resolution of her symptoms. The presence of what signs or symptoms would favor a diagnosis of pyelonephritis over cystitis, and how would this affect management? 1. Fever (<38.0) or chills 2. Nausea or vomiting 3. Flank pain or costovertebral angle tenderness 4. WBC casts on urine microscopy Nitrofurantoin, fosfomycin and pivmecillinam do not achieve adequate renal levels, so the most appropriate empiric antibiotic choices in pyelonephritis include: 1. Fluoroquinolone (unless resistance patterns are greater than 10%) 2. Trimethoprim-Sulfamethoxazole (unless resistance patterns are greater than 20%) 3. Extended spectrum beta-lactam (commonly a third- or fourth-generation cephalosporin, but may include medications such as ampicillin/sulbactam or piperacillin/tazobactam) 4. Aztreonam if the patient has a severe allergy or contraindication against the above antibiotic choices MKSAP 16 Questions ID Question 31: Prevention of CA-UTI (Answer - A) ID Question 32: Diagnosis of CA-UTI (Answer - D) ID Question 36: Management of acute uncomplicated cystitis (Answer - D) ID Question 71: Management of pyelonephritis (Answer - B) ID Question 106: Prophylaxis of recurrent UTI (Answer - C) Post Module Evaluation Please place completed evaluation in an interdepartmental mail envelope and address to Dr. Wendy Gerstein, Department of Medicine, VAMC (111), or give to Dr. Patrick Rendon, Division of Hospital Medicine, UNM Hospital. 1) Topic of module:__________________________ 2) On a scale of 1-5, how effective was this module for learning this topic? _________ (1= not effective at all, 5 = extremely effective) 3) Were there any obvious errors, confusing data, or omissions? Please list/comment below: ______________________________________________________________________________ ______________________________________________________________________________ ______________________________________________________________________________ ______________________________________________________ 4) Was the attending involved in the teaching of this module? Yes/no (please circle). 5) Please provide any further comments/feedback about this module, or the inpatient curriculum in general: 6) Please circle one: Attending Resident (R2/R3) Intern Medical student